So I had the great honor of attending the World Federation for Laser Dentistry (WFLD) 2024 event in Sao Paulo, Brazil, a few days ago. Overall that event was amazing but there were a few downsides as well! In this article I'll guide you through my experience and showcase the most important lessons I've learned from the event.
It was wonderful to meet so many dentists who use light therapy. Dentists with all types of backgrounds were at the event, such as those who are in clinical practice, academics, and various people involved in the development of the laser technology.
In this case, lasers predominate dentistry–not the LEDs you're probably more familiar with that I and others of our brand cover so often. I'll comment on this topic later.
And, just so you know - I was invited to this event by my good friend after I wrote my PBM (PhotoBioModulation) 2024 article. But, as I don't have a background in dentistry, I used the months of September and October to read up on the latest science on this topic. So before the WFLD 2024 event, I had to take a tour de force through all of the most important topics - such as light therapy for periodontal disease, dentin hypersensitivity, oral surgery, and so forth!
- Red Light Therapy For Oral Health Ultimate Guide: 20 Unique Benefits!
- Dentin Hypersensitivity: Why Red Light Therapy Is A Game-Changer
- How Red Light Therapy In Dental Anesthesia Practices Shows Great Promise
- The Remarkable Role Of Light Therapy In Periodontal Care
- Dental Red Light Therapy Before And After Case Studies From Clinical Practice
- Oral Wound Healing With Red Light Therapy: Innovative Advancement?
I think I reasonably succeeded in getting a good overview of light therapy for the dentistry field. So, I went to the beautiful Sao Paulo, Brazil - my second time in the city!
And, as always, I loved the culture there. I just love Brasil and that will never change! I want to thank everyone for the beautiful time, but in particular, Professor Aldo Brugnera and Professor Samir Nammour for inviting me there, my great friend Dr Ana Paula Tanko for the incredible hospitality, and Prof Reem Hanna for the wonderful conversations.
Brasil has captured my soul, and very soon, I think I'll be coming back again! This is, from a person speaking who has lived in Rio for 3 months...
Next up I'll say that I've tried to cover as many of the topics as I could. But often, 3-4 different presentations on different topics were held at the same time, meaning that you cannot physically attend all of them.
Lastly, I've tried to make this article accessible to a broader audience - the average person who isn't aware of how light therapy is revolutionizing dentistry. Even I wasn't aware of that process before I started reading up on the topic two months ago.
But, as it turns out, Vladimir Heiskanen's Excel sheet that contains most photobiomodulation (PBM) studies contains 1,800 studies on light therapy for dentistry, which are about 20% of all available studies in the PBM field right now. So, laser dentistry, and PBM in general, is barely a fringe development. And, the number of publications is exponentially increasing, meaning that this field will become more important with time!
Why?
Let's find out below...
My only regret is this: I could have created 15 or 20 or even 30 lessons based on the experience in Sao Paulo. I just didn't have the time to attend all speeches and gather all knowledge. So in reality, event though this is a 10,000-word blog post, it should have been double or triple the size for full justice!
I know all of you people work hard. I could have created a 20,000 or 30,000-word blog post based on what I saw but I restricted myself to 10,000 words! I hope you enjoy the show! I'm very sorry to all the fantastic scientists who made a vast contribution to light therapy and dentistry, which I didn't cover in this blog post!
If you need an introduction into what these terms means, check the following resources:
- What Is Red Light Therapy?
- Red Light Therapy Explained: Basic Terms Guide
- Start Here - Light Therapy 101 & Buyers Guide
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
- How Often Should You Use Red Light Therapy Explained
These resources should give you a basic understanding of how red light therapy works, and the discussions around it!
Lesson 1: Photobiomodulation For Oral Health Simply Works
After meticulously citing dozens of studies on different topics of photobiomodulation for oral health, I'd get feedback from dentists themselves in our Facebook group that "this must all be a placebo" and that the dentist "has never seen any other dentist use light therapy in their daily practice".
Well, sure! But the fact that a therapy hasn't found widespread adoption yet, doesn't mean it doesn't work. Once upon a time, there wasn't any anesthesia in dentistry. That changed, and dentistry was never the same.
The same is true for light therapy in dentistry. Now, the most important reason why the amount of research in this area is exploding is because study participants and patients get excellent results. Some of these results are hard to believe for both dentists and outsiders.
When I looked at light therapy for dentin hypersensitivity, I found that study participants have 40 - 70% pain reductions on a VAS ("Visual Analogue Scale) scale that measures pain from 0 - 100. At most, a few sessions are needed to achieve these results. And the results also last for months - as long as the researchers are generally able to track participants!
And when applying light therapy before using an anesthetic needle for dentistry interventions, you'd get 20 - 40% reductions in the injection pain on that same VAS scale. At the maximum, you'll only need a minute or two of treatment for these results. Pain and the fear of injections is one of the most frequent reasons people avoid the dentist in the first place, so this development is huge. And, the process also works in kids - so light therapy could redefine what going to the dentist means on a psychological level, for kids, based on this development alone.
There are tons of other examples that I will venture into later...
Nevertheless, the reason light therapy in dentistry is exploding is because the results are almost too good to believe. In the rest of this article, I'll give you many examples of these developments!
I'll try to minimize mentioning the specific type of laser and will focus more on the light therapy wavelength, to make it more accessible.
CO2 lasers, for instance, have wavelengths around the 10,000 nm-mark, such as 9,300 and 10,600 nm. That CO2 laser is great for surgical procedures on soft tissues, such as removing excess periodontal (gum) tissue for aesthetic purposes and managing soft tissue lesions.
The Er:YAG (Erbium with a yttrium-aluminum-garnet, emits light at 2,940 nm. Prof Akira Aoki had an excellent presentation on the use of the Er:YAG laser (1). That laser can be used, and I quote, for making an "incision, flap elevation ["pulling" your gums higher so they cover the tooth better], root debridement [removing biofilm and tartar from your teeth], bone defect debridement [removal of defective bone, among others], ostectomy, decortication [removing jawbone tissue strategically], blood coagulation and activation, [and finally a] releasing incision". As you can see, these are primarily surgical procedures whereby a higher nm near-infrared wavelength is beneficial!
Prof Akira Aoki argued that the Er:YAG lasers is a great assistance to traditional periodontal surgery - especially given that new techniques will be developed here! The Er:YAG laser can also be used to lower inflammation and boost wound healing, however.
Other lasers are also used, such as argon lasers at 488 and 514 nm, mainly for tooth whitening and the coloring of dental compounds. The Neodymium laser (1,064 nm), diode lasers (810, 940 and 980 nm), and . Helium-Neon (HeNe) laser (632 nm) provide wavelengths that are far better known in the red light therapy space. These lasers are used more for restorative purposes, as you are familiar with in the red light therapy space!
The most important information to remember here is that various lasers exist, with different effects depending on the wavelength. Wavelengths above 1,100 or so are often used for soft and hard tissue surgery. Lasers emitting light between 600 and 1,100 nm are often used for general health support (photobiomodulation), but there is no hard rule here. The problem with universal rules here is that even an 810 nm laser can be used for cutting tissue at high power.
Many different laser variations exist. Other examples are the Nd:YAG and Nd:YAP lasers. In the first, the Yttrium Aluminum Garnet (YAG) crystal is used which I mentioned before. In the second, the Yttrium Aluminum Perovskite (YAP) is used. Both are doped in Nyodeum ions. While it sounds complicated, the most important thing to remember is that the Nd:YAG operates at 1,064 nm, generally, and the Nd:YAP at 1,340 nm. These wavelengths can differ though.
For the average person, it's most important to understand that the materials of the laser and by changing its configuation, you can change the wavelenght emitted! The amount of energy you put into the laser (Wattage) co-determines the quantity of light (power output) is emitted.
Lesson 2: Professor Samir Nammour Teaches That Light Therapy Plays An Integral Role In Caries Prevention
Let's not deceive ourselves: if caries can be prevented in dentistry, we'd have won half the battle! And, Professor Samir Nammour. Professor Nammour has quite a few publications on the topic of caries and light therapy (2; 3; 4; 5; 6). Professor Nammour has been in the laser dentistry space for around four decades now and is a veteran in the field!
I also want to thank Prof Nammour for the wonderful interview on the role of lasers in dentistry and its history - subscribe below if you're interested in following that:
But let's consider the role of light therapy in relation to caries. Professor Nammour's talk was aptly titled "Laser progress in caries prevention."
First of all, Professor Nammour emphasized that caries prevention specifically and oral health in general is a multifactorial process. I've mentioned that fact before, in my dentin hypersensitivity and periodontal health articles. I quote Prof Nammour's identified factors from his presentation sheets below:
"1. Poor oral hygiene
2. Dental Plaque formation (Biofilm)
3. Excessive sugar consumption
4. Composition of Enamel Stucture
5. Enamel malformation & development of defects
6. Low fluoride intake"
Eventually, the hydroxyapatite crystals of your teeth (the calcium-phosphorus connections) make up almost all of the enamel. The enamel is the hard outer layer of your teeth. The dentin contains lots of hydroxyapatite too, but less so than the enamel. The dentin is the second layer of the teeth - shown here:
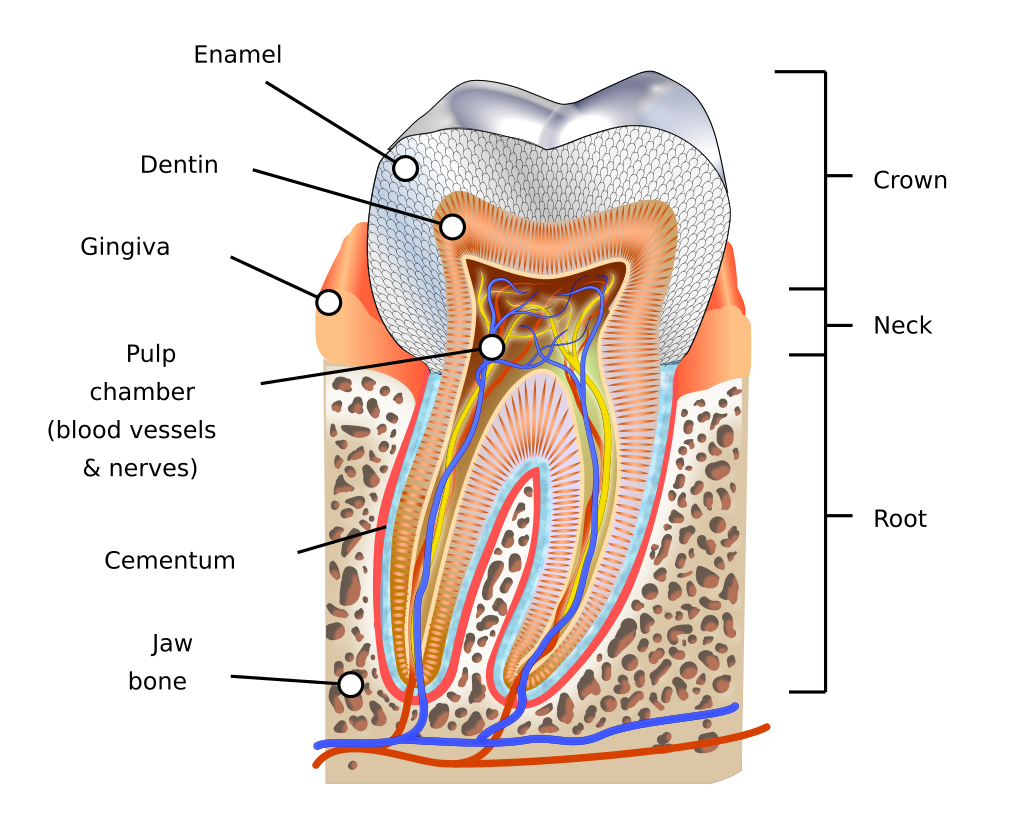
The key here is preventing the enamel and dentin from degrading. Once the pulp is affected, you'll be met with the characteristic shooting tooth pain!
During the talk, I was pleasantly surprised by Prof Nammour's insistance that excess fluoride exposure can be toxic.
(I think that fluoride probably has no positive role after looking at the research, especially since hydroxyapatite is now available and shows similar tooth-hardening results in dentistry.)
Nevertheless, the most important finding of Prof Nammour is that "previous studies have recorded the reduction of caries-like lesions by lased enamel". So, by dentists applying light therapy, you lower caries risk.
Different lasers can be used for that process. The lasers have two effects here. First, there are physical changes that lower the permeability of the enamel. Imagine your enamel has a higher density, like a rock that becomes harder.
Secondly, chemical changes are reducing the solubility of the enamel. Here, you can imagine the outer layer of your teeth is more resistant to insults from sparkling water with lemon juice or the effects of microbes in your mouth after you consume a sugary drink.
Also, fluoride is better incorporated into the enamel, according to Prof Nammour. So, if you are a proponent of fluoride in dentistry (everyone is free to be so), then laser therapy can improve the effectiveness of your therapy!
The result is an improvement in the structure of your teeth's enamel, making them more caries-resistant. Low-energy lasers the tool of choice here, not higher-powered lasers. Higher-powered lasers can cause "crack formation" which is avoided with lower-density lasers.
This conclusions accords to that of my own. As a general pattern, for health support lower power outputs and total doses (measured in J/cm2) seem to have better effects in light therapy for oral health!
It's wonderful to see that more tools are developed in dentistry to prevent caries. Because, if you can prevent a problem from arising in the first place, many other dental interventions, whether it's drilling, root canals, or tooth extractions, are far less likely to be needed in the long run! It's my belief that both hydroxyapatite and light therapy will revolutionize caries prevention in the next decade (perhaps, with an awareness of mouth breathing risk as a close third!)
For the best results, seek out a dentist with experience applying lasers for dental care. That dentist will guide you in caries prevention!
In Prof Cassoni's studies high-power lasers were used at low doses for the prevention of caries. These are CO2 and Erbium lasers. Current systematic reviews, however, assume that there's currently too little evidence to recommend universal application of light therapy for caries.
Prof Cassani made the case that so-called "secondary caries" are a huge problem in dentistry. Secondary caries happen when a cavity is corrected, but later on, caries form under the correction. The correction here can be a cavity filled with resin, but also a crown place on a damaged tooth, and more. The problem here is that these caries are very hard to identify, let alone reach. Fortunately, laser therapy may play a role in countering these hard-to-treat and identify secondary caries!
Lesson 3: Revolutionizing Oral Microbiome Care With Light Therapy By Professor Kinga Grzech-Leśniak
With light therapy, you don't just have a benefit for caries prevention. Perhaps the even bigger revolution exists in changes of the oral microbiome by applying light therapy, which then have benefits across the board for not only your oral health but also overall health.
The oral microbiome has taken a vital place in both oral and systemic health in the last decade (7; 8; 9; 10). The oral microbiome, just like your gut microbiome, likely plays a role in many systemic diseases - although research here is still in its infancy (7). That microbiome also plays a major role in periodontal disease, which then plays a major role in systemic health (8).
I quote from my work on periodontal health here when looking at how risk factors of other diseases increase with periodontal disease:
""all-cause mortality," or your overall risk of dying independent of cause by 46%
- diabetes and cardiovascular disease - with a 15 - 47% increase in a "coronary heart disease event" such as a heart attack with periodontal disease (depending on the study)
- stroke, in particular, cerebral ischemia, with a 60 - 330% higher risk with (severe) periodontal disease. The worse the periodontal disease, the higher the risk here.
- Alzheimer's disease
- adverse pregnancy events of 77%
- a few cancers, such as colorectal cancer (45%) and oral cancer, as well as overall cancers by 38%
-Rheumatoid Arthritis
- chronic kidney disease, where the risk in some studies is very small and in others by 100%
- respiratory illness
- And, most importantly, poorer overall oral health! So the worse your gum and adjacent tissue's health becomes, the worse many other issues in your mouth become!"
The oral microbiome itself has also been linked to respiratory disease, heart and blood vessel issues, metabolic conditions, Alzheimer's Disease, and Rheumatoid Arthritis (9). Optimizing that oral microbiome likely has huge effects on disease risk and overall health (10). I fully expect the oral microbiome's influence to gain more prominence in the coming decade(s), just like the gut microbiome did.
But after this short introduction, let's return to the topic of light therapy. Professor Kinga Grzech-Leśniak has done some groundbreaking research on the interaction of light therapy and the oral microbiome (11; 12; 13; 14; 15; 16; 17; 18; 19).
In her presentation, Professor Kinga Grzech-Leśniak showed dramatic reductions in periodontal pathogens with light therapy applications. An example she gives the P. gingivalis, a bacteria involved with periodontal disease. Pathogens have reductions in their numbers across the board.
Some in vitro studies show reductions of 85 - 95% in bacteria (11). An "RCT" study shows that Photo-Dynamic Therapy (PDT) - whereby a compound is used that is sensitized by light - can reduce bleeding and the microbiome of the mouth (12). In vitro here means "in the glass", which are the foundational studies you did in science class. RCTs - or Randomized Controlled Trials - use a control (placebo) and intervention group to test the effectiveness of an intervention.
Another of Professor Kinga Grzech-Leśniak's studies finds the following data:
"The combined NdErNd laser (93.0%), followed closely by Er:YAG laser (84.9%), treatment resulted in the highest reduction of all bacteria count after 6 months, whereas [Scaling and Root Planing] (46.2%) failed to reduce Treponema denticola, Peptostreptococcus micros, and Capnocytophaga gingivalis. Full-mouth plaque and bleeding on probing scores dropped after 6 months and were the lowest in both laser groups." (13)
So, standard scaling and root planing led to an almost halving of bacteria count because of the cleaning below the gum line. But, light therapy led to much bigger improvements, of up to almost 95% reductions (when different lasers were applied) that were far better than traditional mechanical cleaning methods!
Yes, there are improvements in these domains with scaling and root planing, too. But light therapy seems to be super effective in comparison! The big benefit here is that the laser can be applied without the side effects of the traditional methods. So you can specifically target the bacteria in the mouth only, often combined with PDT, without negatively affecting the periodontic tissue.
Different compounds can be used for that PDT, such as sodium hypochlorite and hydrogen peroxide. And, yes, more high-quality RCT studies are needed here but the results are extremely promising!
And yes, Grzech-Leśniak admits that periodontitis is multifactorial. However, a poor oral microbiome is one of the main factors here, and light therapy directly targets it. The end result, however, is not just an improvement in the microbiome but also in two other important outcomes, 1) pocket depth; 2) the clinical attachment level.
Clinical attachment level is how high the gums attach on your tooth. With more severe periodontitis, this problem worsens. Pocket depth is how deep of a separation there is between gum tissue and your tooth -
Suffice it to say, I'll be following Professor Kinga Grzech-Leśniak's work very closely! But I hope you're beginning to see the pattern I talked about in lesson 1: light therapy in dentistry is huge. There are very spectacular results with caries and periodontitis, two of the biggest preliminary problems that spiral out of control for many people all across the planet, over time. If only these two results were available from light therapy, it would already be revolutionary.
Professor Theodoro showed a great list of photosensitizers in her presentation of different compounds and what light they react to, that I'll quote here:
"Methylene Blue (610 - 660 nm)
Toluidine Blue O (590 - 630 nm)
Rose Bengal (480 - 600 nm)
Chlorine (440 or 660 nm)
Erythrosine (400 - 550 --blue or green)
Rhodamine (450 - 590 nm)
Phthalocyanines (660 - 700 nm)
Curcumin (420 - 460 nm)
INdocyanine green (infra-red)"
It's very interesting to see that so many compounds can be used for aPDT! You can just randomly use them, however, as the dose, the time or pre-irradiation, and other factors play a role.
Another problem in periodontal treatment in general, with lasers, is that there's no universal dosing protocol. Nevertheless, aPDT likely has a strong future because it's cheap to apply and comes without side effects. Other means of impairing microbes, such as antibiotics, can create problems over the long term. If more aPDT was used instead of antibiotics, as the gold standard treatment, fewer antibiotic-resistant bacteria would emergy
Prof Theodoro prefers a lower methylene blue dose when applying aPDT for periodontitis. That PDT is applied for five minutes and then 660 nm light is applied in the periodontal pockets. Right now, Prof Theodoro has achieved great results in rat studies--so human studies are needed for confirmation.
Impressive! But there are many more results...
Fasten your seatbelts:
Lesson 4: New Laser Technologies & Applications With Professor Aldo Brugnera
First of all, I want to thank Professor Aldo Brugnera for being so nice to invite me to the congress in Brazil! The congress was a big success, in my opinion - especially as a newcomer to the space.
Professor Brugnera also gave me the honor of interviewing him, just before he gave the final main speech of the conference. That interview will be uploaded to our YouTube channel as soon as possible, so subscribe if you don't want to miss it!
One of Professor Brugnera's messages during both my interview and his speech was that there are two main areas where the scientific developments are really exciting to him:
- The correction of "black spaces in the interdental papilla" - which is complex wording for people who have incomplete gum tissue covering between the teeth. As a result, you can look between the teeth into the oral cavity. Here, apparently, gum tissue can be regenerated if the correct procedure is applied (20; 21; 22; 23). This research does seem more in the initial stages, but is once again extremely promising. Prof Brugnera carries out much of that research with his wife, Prof Fatima Zanin.
- The removal of products used for dental aesthetics with lasers, such as veneers. The benefit here is that there are no side effects, compared with traditional methods!
- Light therapy has a strong effect on peri-implantitis - inflammation around implants that have been placed. I'll come back to this topic later. Nevertheless, a common problem with implants is that they cause issues with the tissues around them. And, once you've got chronic inflammation in the area the implant, it's also hard to treat. But lasers may change that - with laser therapy there are improvements in the amount of bleeding, pocket depth, clinical attachment level, bone filling and the extent of the bone gain. Bone and gum loss around the implant can become a problem and laser therapy seems to counter both!
On a related side note, Professor Brugnera hosted a wonderful gala at the second night of the 3-day conference. The food was wonderful there, and the Brazilian music and dance were even more wonderful! Some people only felt that the party should have continued longer (Brazilians!), but I think the choice was strategic as otherwise nobody would show up for the third conference day...
Professor Shibli and his collaborators have published very extensively about that topic for many years so he's a true expert in the field (30; 31; 32; 33; 34; 35; 36)!
Current strategies include mechanical and physical debridement and antimicrobial agents. Physical debridement can happen with a laser or mechanical dentist tools. Antimicrobial agents not only include antibiotics here, but also aPDT - which I'll come back to later!
The problem here is that 20% of people end up with peri-implantitis. And, over time the problem is hard to fix and often escalates. The 20% figure doesn't sound too bad - because it's only a 1/5 change, right - until you realize that's per implant. So, the risk dramatically goes up the more implants you have in your mouth.
Also, the big issue with implants is that traditional periodontal strategies don't work. For instance, scaling and root planing that removes tartar and bacteria from under the gumline cannot be applied. So you need other strategies here!
According to Prof Shibli, 40% of implants end up with inflammation after five years. And, lasers seem really promising here for dealing with that inflammation, even though much more high-quality research is needed. Many Randomized Controlled Trials that are currently published, use the incorrect treatment parameters and therefore don't achieve the intended results.
Professor Shibli has a few conclusion, and I quote:
"1) Treatment of peri-implantitis is a hard task (with or without lasers!)
2) [A d]etoxification process is sine-qua-non to achieve a better environment for new osseointegration or re-osseointegration
3) High-power laser could improve clinical outcomes [if] they are used in the right way
4) Further studies comparing different clinical endpoints for the resolution of peri-implantitis could help established personal peri-implant treatment guidelines"
So, there is a lot of promise but also lots of work to be done!
Lesson 5: The Research Will Lead To New Consumer And Non-Consumer Based Products
So, I've got a dilemma. On the one hand, I'd love to "democratize" the use of light therapy in dentistry as much as possible so that it's available for a broader audience. My good friend Alex Fergus has already reviewed a few devices, such as the LightpathLED Diesel Torch which has an oral attachment. Check Alex's review here:
Then there's the Noovalab Novoral Care product that Alex has reviewed here:
Ideally, the consumer would have access to many different light therapy products for various oral care goals. However, the big issue is that it's not recommended that consumers themselves apply light therapy for every case. Applying light treatment, in many cases, carries an inherent risk.
Think about removing the veneers from your teeth with a high-powered laser that I talked about in the previous lesson. Would you be comfortable removing your own veneers, with the risk that if you got a setting wrong, you may damage the underlying tooth? Likely not...
Also, the light therapy that's used in conjunction with periodontal interventions is probably best applied by a dentist. Tooth extractions are another example, as is managing the peri-implantitis I talked about before.
Sometimes, you just want a medical professional to apply the therapy because they've got extensive experience with it. One of my dentist friends, Dr Ana Paula Tanko, uses light therapy with every patient in her practice - systemic light therapy at the very least, and local light therapy where applicable.
However, I also see the development of more consumer-based LED devices in oral care. The two products I've mentioned above are some of the first popular ones on the market right now. For some goals, such as caries prevention or optimizing periodontal health, low-powered products will likely be more widespread available in the coming years.
And that's a good thing!
What matters here is that applying light therapy can have an inherent risk. Some higher-powered lasers are used for soft and hard tissue surgery, for instance, and you don't want the average person to carry out these procedures themselves. Yes, that conclusion is a bit common sense and nevertheless important to spell out!
Examples of consumer-applications I envision become more popular in the future are bone repair (with standardized protocols, just as with eye health), burning mouth syndrome, dry mouth, nerve repair, TMD/TMJ (jaw disorders!), orthodontics, oral mucositis, and a few more! But, for surgery such as endodontics, lasers will arguably always be used by a dentist specialized in light therapy - due to the inherent risk.
But just as dentists tell consumers that they should floss and brush their teeth, hopefully in a 5 or 10 years from now we can recommend inexpensive lower-powered LED devices to consumers. And, with these LED devices consumers can then reduce their caries risk and improve periodontal health.
Given that many studies here used lower-powered interventions, I'm very hopeful about that prospect!
Lesson 6: Tons Of Great Laser Products Are Hitting The Market - And Brazil Is The Innovative Wild West!
Brazil is among the top nations in the red light therapy ("photobiomodulation") space, as seen from the number of publications. What's also remarkable is that Brazil has a much freer perspective on light therapy than in the West, such as the US and countries in the EU.
Talking to some people in congress, I learned that there's much less regulation for using lasers even than in most other countries. In that regard, Brazil is the Wild West. And that Wild West comes with both risks and opportunities.
I learned that you can just buy a medical 5 Watt or even a whopping 15 Watt laser from a company and use that on patients, with minimal training. In the US and EU, people are generally forced to undergo mandatory training before using such products. But in Brazil, anything is possible.
Of course, if you hurt a patient, you'll still be medically liable so there's every incentive not to "experiment" with anything crazy. I was just astounded that such products can be used without much formal training.
Why?
One example here is Cromatic from Brazil which has an impressive lineup of lasers:

These lasers have many different medical applications–not just for oral care. These can be used for tissue repair, for instance, and some of the higher-powered lasers can even be used for tattoo removal.
When using the Lumière device, which operates at a maximum of a whopping 15 Watts, I could see the smoke coming from a piece of paper. And that smoke occurred far from full power. So you can hurt people with such devices if you don't know what you're doing!
(Which proves my earlier point of lesson 5!)
The downside here is that many of the products from Brazil aren't internationally available. Cromatic offers multiple products and they come at a higher price point, with the Lumière coming in at as much as $45K USD I think! So these are mostly made for medical professionals working in clinics or medical settings.
What I liked about the Cromatic devices was how well they were designed, how good they looked, and how you could adjust treatment parameters to incredible detail through the touchscreen. You can adjust anything from power output, pulsing frequency, beam area, and more.
This device is at the level of what many US companies offer, but with greater customizability in my opinion. Of course, that customizability is both a risk and an opportunity!
Lesson 7: Optimizing Dosing With Professor Reem Hanna
I had seen Professor Reem Hanna's presentation during Photobiomodulation (PBM) 2024. That presentation really got me interested in light therapy for dentistry. A few weeks after PBM, I began a very rigorous preparation period of reading and writing articles on light therapy for dentistry - to prepare for the WFLD 2024 event! So thanks, Prof Reem, among others, for inspiring me!
Professor Hanna first talked about a study she published years ago about the stimulating so-called "osteoblasts" in relation to dosing (45; 46). You may know that I've got a hate-love relationship with this topic, as readers always question me about dosimetry (or "dosing" in plain English) and I cannot give them simple answers. Hence, I wrote two extensive articles about dosing that you can find here:
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
However, my conclusion, that there no simple answers and that there are not a few simple laws, like in Newtonian mechanics, that can predict and explain all phenomena.
My argument there is that biological creates are complex systems (organisms), where, the parts and the whole interact in dynamic ways that cannot be reduced to simple mechanistic laws. This conclusion is unfortunate as it doesn't allow us to simplify red light therapy (or "photobiomodulation") dosing, and yet, it is correct in my opinion. I do hope, of course, for a Newton to give us a few simple laws of photobiomodulation as it would make all our lives easier!
But back to Hanna's important research:
Hanna's study compared a flat-top beam with a Gaussian-beam profile. The flat-top beam has a more even distribution of light, and the Gaussian beam a bigger peak in the middle. If you've got some background in statistics, you can imagine a Gaussian distribution curve with a more flat curve. By comparing the two beam configurations, Hanna hoped to learn whether a more peaking beam (Gaussian) or more even distribution of light (flat-top) worked best.
Both beam configurations used 980 nm. The study used a power output of 900 mW/cm2 into a cell culture (in vitro), for 60 seconds to achieve a total dose of 55 J/cm2.
But let's take a step back...
The osteoblasts mentioned before, are involved in creating bone materials. So, stimulating osteoblasts anywhere in the body can improve bone repair and formation. Prof Hanna's question and that of her team of researchers, is what beam profile best stimulates osteoblast formation.
More broadly, if there's a difference in outcomes in these two beam configurations, it means that distributions of light influence the final treatment outcome. And, if the treatment outcome is influenced by the light distribution, then you'll have to account for it in your treatments. So this in vitro study is not merely an intellectual curiosity but instead has implications for the daily application of lasers to patients.
So, what was the outcome?
Although I'm oversimplifying here, it turns out that the flat-top has some benefits, in that pre-osteoblastic cell formation was better. Hanna and associated researchers have identified biological mechanisms for this process, stating that this happens
"through activation of Wnt signaling and activation of Smads 2/3-βcatenin pathway." (45).
It's far more complicated than what I'm showing here, however, as the different beams were also tested at different distances (46).
Hanna discussed more interesting research in her presentation, such as a paper on mitochondria - a study in which she participated (47). The study also concerns dosing or dosimetry. I'm oversimplifying here, but mitochondria were removed from rats and isolated. The mitochondria were then irradiated with different power densities. The researchers ensured a pure experiment as much as possible, trying to account for scattering, reflection, light absorption, and so forth.
The key outcome here was that a 0.8 - 1.1 W dose optimized for ATP production and improvements of complex III and IV at the mitochondria. Complexes III and IV both participate in ATP production - ATP is the main "currency" or "unit of account" for energy production in the body. After complex IV, the energy-creation process is complete and the oxygen you inhale is transformed into water and CO2 (as well as energy and other byproducts).
These dosing studies are necessary to understand what happens at the cellular level with different doses of light. By knowing better what happens with the light at the cellular (or better yet, "mitochondrial") level, you'll get a better understanding of dosing in humans, eventually.
Professor Reem made many arguments I cannot 100% follow based on her presentation. I cannot break them all in full detail here! Suffice it to say, that Professor Reem has made great contributions to light therapy dosing!
Lesson 8: Promoting Better Protocols For Periodontitis And Peri-Implantitis With Professor Preetinder Singh
Sorry everyone, but Professor Preetinder Singh was the coolest guy at the conference! Prof Singh is real funny and has a wonderful relaxed way of presenting his work. In the spare time, and during the Gala and other events, he's even funnier!
But let's get real:
Professor Singh has extensively thought about what is called "LANAP" and "LAPIP" - updated treatment protocols for periodontitis and peri-implantitis. It was harder for me to find his publications on this topic, however, but his presentation showed great insight (24; 25; 26).
So why pick lasers according to Prof Singh? Well, it's less invasive than traditional mechanical methods. With an Nd:YAG laser (1,064 nm), in this case, the LANAP procedure allows for the better attachment of gum tissue.
"LANAP" stands for "Laser Assisted New Attachment Procedure" - although it's not really new because it's from the 1980s now. Here's how it works - I'm paraphrasing Prof Singh's sheets:
- You probe the pocket depth of a gum.
- You then use the laser in the pocket to vaporize diseased tissue.
- You mechanically excess remove tissue from the root of the tooth with a scaler device.
- Bone structure is optimized with that scaler.
- Then, you use a laser again to form a fibrin clot. That clot stimulates the healing!
- Using the fibrin clot, the gum tissue is reattached higher up the tooth.
- Over time, this tissue heals and you've now got the gums reattached at a much better position than before the procedure!
- This procedure has to be carried out by a dentist, because of the mechanical scaling that's involved–you cannot try this at home! You also need a high-powered 4W laser for this procedure that is potentially dangerous and harmful if misused (27). The procedure is also complex and can involve medication such as antibiotics and other dental procedures. You also need to be trained in LANAP before you can apply it!
It's easy to imagine why the LANAP would work for many people, as the loss of gum tissue and the attachment level is the foundational problem in periodontal health.
Why does LANAP work? Prof Singh gives the following reasons - I paraphrase again (27):
- Only diseased tissue absorbs the laser, while adjacent healthy tissue remains unaffected.
- Bacteria and other microbes are killed in the area that cause the inflammation.
- The fibrin clot that forms acts as a barrier, preventing new microbes from entering the previous periodontal pocket.
- The gum tissue heals from the bottom-up, inside-out, and has now much better coverage around the tooth!
Next up, Prof Singh discussed "LAPIP," or the "Laser Assisted Peri-Implantitis Procedure." About 20% of implants placed develop inflammation - called "peri-implantitis". The 1,064 nm wavelength can help here, once again, with the Nd:YAG laser once again.
Professor Singh also discussed a few other interesting topics, such as "superosseointegration" and the BLAST implant protocol. The latter is a protocol to better help integrate implants after they've been placed. The benefits of that BLAST protocol allows for quicker healing and recovery, less pain, and a higher success rate of oral implants. And because of the many reasons I've mentioned before in this article, higher success rates are very much necessary!
BLAST stands for "Bi-axial Loading At Specified Torque". The goal here is to create a very precise implant and placement of that implant for perfect stability. The implant is also placed in such a way to minimize stress in the underlying bone. Imaging techniques ensure that the placement is optimized. Even the placement of the implant itself is carried out in a very controlled manner to avoid damage. In the end, the BLAST protocol minimizes the risk of having issues with your implant, such as peri-implantitis or instability or underlying bone issues.
Light therapy can guide that entire process. Pre-treatment, for instance, you can ensure better health of the gum and bone tissue. And after implants are placed, light therapy can boost the recovery process. UV desinfection can play a major role as well, here, to minimize the risk of microbial issues!
I know a few people in my personal life who have either early or advanced periodontal disease. But, even though the LANAP protocol has been around for four decades now, they've never been offered that treatment in my home country in the Netherlands. The Mexican dentists who I've visted - even biological dentists there - are also woefully unaware of the effects of light therapy on oral health!
Lesson 9: Improving Facial Aesthetics With Associate Professor Patricia Moreira de Freitas
Associate Professor Patricia Moreira de Freitas gave a great presentation on how light therapy can be used to enhance skin beauty (37). I've written about the topic of light therapy for skin beauty before so I'm familiar with the topic.
In a way, aesthetic dentistry and facial beauty go hand in hand because they mutually support each other. You wouldn't want to have perfect skin with very poor-looking teeth, or vice versa, right?
Well, Professor Moreira de Freitas did discuss a very important topic that has been haunting us at Light Therapy Insiders for more than a year now! Ever since PlatinumLED has come out with a BioMax range with wavelength in the 1,000+ nm range, people have been complaining about facial fat loss. Correct or not, we've taken these claims seriously.
And, it turns out that Professor Moreira de Freitas does have a way to stimulate facial fat loss, but only under very specific circumstances. Here, a 1,400 nm laser will be inserted directly through the skin, into the subcutaneous tissue. This process then leads to fat loss.
The high-powered lasers are specifically used for lipolysis and/or endolifting - so the removal of fat tissue from under the skin. To me it's extremely unlikely that this effect can be achieved with low-powered lasers, let alone red light therapy panels that you use from a distance.
Light just really works differently at different power outputs. So, 810 nm light from a panel at a 12-inch distance works totally different than if you'd use a 5 Watt laser at 810 nm in a very small area!
But let's get back to the facial fat loss. Of course, there are many situations where you may want to stimulte local fat loss, such as in the face. An example is if you hold excess body fat in your face - locally removing that body fat can dramatically improve your looks.
Getting closer to a perfect amount of facial fat very quickly enhances your overall appearance. I myself know, because I look far better at lower body fat percentages than higher ones!
With regards to beauty, the innovation here is that different wavelengths are now tested for and used (38). And new lasers are also tested and sometimes combined with cooling technology to prevent heating of the skin.
Next up, Professor Moreira de Freitas talked about a few other applications for enhancing facial beauty, such as Botulin Toxin (Botox) combined with red light therapy (photobiomodulation). Both apparently have synergistic effects - although I still have to try! So if I look 10 years younger during next year's WFLD congress, you know why...
You first apply the Botox into the face (don't do this at home!). Then, a 890 nm GaAs laser is used for a total dose of 16 J/cm2. That dose is applied in 40 seconds, so you'll need quite a powerful device! The light is applied to four different spots of 0.07 cm2. Treatment frequency is ten sessions over three weeks.
Seeing the before and after picture of Professor Moreira de Freitas, the results are well worth it! I'm still surprised at how impactful Brazilian beauty enhancement are.
Professor Moreira de Freitas also gave other examples of how light therapy is applied. One option here is using light therapy after placing fillers in the lips - which also enhance recovery. And, aPDT (antimicrobial-PhotoDynamic Therapy) apparently is very helpful to counter herpes in the lips - we found a similar conclusion because my friend Alex finds light therapy counters herpes big time when he travels:
If you're curious, check out Professor Moreira de Freitas' work - there are many interesting topics covered in her publications, such as light for dental bleaching, orthodontics, research on zirconia (ceramic!) implants and crowns, optimizing the health of the enamel and dentin, and much more (37)!
Lesson 10: Upgrading Clinical Dentistry Cases And Aesthetic Practice With Dr Ana Paula Tanko
So my friend Dr Ana Paula Tanko has an amazing track record. Dr Paula's looks amazing for her age.
The goal here, however, is to improve dentistry outcomes so that you can look great in your 30s-70s! For Dr Ana, who has her clinic in Sao Paulo, Brazil, everything is on the table.
So for my friend Dr Ana Paula Tanko, everything is on the table. Whether you need correction in your breathing areas or teeth, Brazilian surgery will help you. Basic examples here are if a protruding or regressing chin are fixed.
My friend Dr Ana Paula Tanko has achieved the impossible with these practices. The pattern is very clear: If you correct your problems in the facial, oral, and neck area, both your health and aesthetics dramatically improve.
Nobody has influenced my viewpoint about dentistry and light therapy more than her. Dr Tanko has done a wonderful job of translating how corrections in the face and neck area, can improve health. An example here is if you've got improper breathing.
The most important part of orofacial harmonization - as Ana Paula and others in Brazil will call the technique - is that the whole facial, neck, and oral areas is taken into account.
Just think about a building without a proper foundation - it's unstable in the same way a face is when corrected. Of course, all of these developments lead to aesthetical improvements, next to health. This is not just about your health but also about how you look!
(I'll be publishing an in-depth interview about PBM in Dr Tanko's clinical practice soon on our YouTube channel! - so subscribe for that!) Let me say that Dr. Tanko has some great strategies for issues that have been haunting people, such as melasma!)
My friend Dr Ana Paula's philosophy on dentistry and health in general is something we should all emulate. You can look great once you go into your 40s and 50s, and you can even look amazing. I thought one of Dr Paula's friends, Nelia, had the same age at 38. The wonders of Brazil are inifinite!
Very soon, I'll also update an article I did with Dr Ana Paula with more clinical case studies.
Also, if your face doesn't look perfect in the mirror, Dr Tanko can probably create improvements there! Contact her HERE to talk!
Lesson 11: Enhanced Root Canal Treatment Success With Professor Josep Arnabat
So I've got a confession to make. I've been very skeptical of root canal treatments in general, in part because many of the biological dentists who I regard very highly - such as Dr Dominic Nischwitz in Germany - make the case that root canals cannot be done safely (45).
However, Professor Josep Arnabat has slightly changed my mind on the topic. Others at the WFLD conference have contributed to that change as well–although I'm still skeptical as to whether it's possible to use root canals in a 100% safe manner!
Professor Josep Arnabat makes the case, however, that light therapy can dramatically increase the effectiveness of root canals (43). The goal here, as Prof Arnabat himself states, is to remove any irritants from the root canal, then clean, fill, and close that root. Finally, the recontamination of the root should be prevented.
The latter, of course, is easier said than done! The whole counterargument critics of root canals make is that, according to them, root canals can never be fully clean. And thus, you'll at least have a partially infected object in your body, that can leech irritants to the outside environment.
Prof Arnabat makes the case based on studies he quotes that 35% of the area within the canal is never filled up. So traditional root canals have a problem (44). However, Prof Arnabat allocates several benefits to laser therapy that can be a game-changer here - and I quote:
"Currently, the laser can be used in endodontics for these effects:
- Bactericical effects
Reducing the number of bacteria
- Effects on the surface of the dentin inside the root canal
Smear layer removal; open dental tubulus
- Photobiomodulation
- Laser biomechanical proparation is absolutely contraindicated"
So that's the information on Prof Arnabat's sheets. The smear layer, above, is the layer of byproduct that has to get cleaned during a root canal treatment. Opening the dental tubulus may enhance the cleaning process - these tubules can be envisioned as rivers in your dentin and pulp area where fluid can pass through.
Essentially, laser therapy can enhance the effectiveness of many of the root canal treatment steps. Both the cleaning and disinfection process will be better, lowering the risk of root canals. Different lasers can be used for this process. I won't go into protocols here because your dentist should be trained in them if you want to use lasers during a procedure.
Nevertheless, besides the antibacterial effects, there are also benefits for tissue recovery and the prognosis of the root canal treatment. And, potentially, root canal treatments, in terms of irrigation of the root, may be carried out with the laser itself, with the 2,780 nm or 2,940 nm wavelenghts!
I am undecided but I do consider laser therapy a great addion here, if you're going to get a root canal anyway! Nevertheless, lasers clean root canals where bacteria love to live.
And Professor Arnabat thinks that root canals are worth it, if and only if done properly! Prof Arnabat's best argument, in my opinion, is that root canals allow you to save teeth. Teeth can be saved for many years if not decades with a root canal. And, there's little risk in trying a root canal because you can always extract the tooth later and use an implant.
Lesson 12: Honorable Mentions!
There are tons of honarable mentions I won't go into much detail here! Here are some examples:
- Light Instruments has some really amazing tools, at 980 nm and into the higher 2,000 nm range, for dentistry. I'm very sorry for the short mention here
- DMC Lasers Brasil also has a great setup, with the wonderful Albert Einstein-like Andre who has a degree in Physics. I learned a lot from Andre!
- Many other people's presentations that I've followed but cannot mention here! I'm very, very sorry I didn't cover you in my article!
Conclusion: WFLD 2025 Romania, Here We Come!
So, yeah, WFLD 2024 was an astounding success! Of course, I would have gone to Brasil anyway if given the opportunity as I've lived in Rio de Janeiro before for a few months in the past and will do so again in the future!
(Now living in Asuncion Paraguay–don't hate me too much, Brazilians! Things just work around here like in Europe ;))
Overall, my conclusion is that light therapy in dentistry - and I use that word "light therapy carefully" - is really underappreciated. Whether the amazing professors of the WFLD want it or not, in the coming years, a shift will be made away from lasers to LEDs, like we've seen in any other market. That shift is already underway for joint pain, brain health, and other areas.
My prediction is that we'll see more LED products in the coming years. But, basically, even if LEDs weren't on the market, I still think light therapy would transform dentistry.
Light therapy has too many benefits to think it's a mere coincidence that it's working. Instead, we should consider light exposure for our oral cavity and surrounding areas as a primordial keystone to our oral health. There should be a shift away from thinking about light therapy as a cure if you've got a condition and a move towards light therapy as health support.
For me, as an outsider, that's easy to conclude. For people in the dentistry profession, that's harder to envision but still ineviatable. Of course, some dentists already envison light therapy as the "alpha and omega" of their practice but currently, if I had to guess, that percentage is rare!
Professor Brugnera does a wonderful job promoting light therapy for oral care. I do have a few points of criticism as well, with first and foremost:
- Many of the lectures weren't available in English. I can understand Brazlians (let's not call it Portuguese ;)) a little bit because I live in LatAm. But most people flying from Tokyo or Eastern Europe won't understand a word and they're fucked, basically! People who travel thousands of kilometers should have their presentations in English, just like I need to adapt to Spanish living in Asuncion Paraguay!
- The gala was amazing. Some Brazilians thought the gala should have lasted longer into the night (not me!). I have to mention this point. Of course, I understand Professor Aldo here in that nobody would show up the next day if the party continues until 3 AM! But my first criticism is the best - just force people to talk in English if you invite international speakers. The same could be done in Poland in 2023, from what I've heard.
Overall, as you can see by the many lessons I've learned above, the WFLD event was amazing! As a guy who has two philosophy degrees, I try to reflect on that. Just like PBM 2024 had to adjust to the advent of laser technology, dentistry needs to accept that too.
In the coming years, many new products will be released regarding light therapy for dentistry. Dentists won't like all of these developments.
But some of these developments will stick and stay around. And some of these developments will still be around in 2030 or 2050.
Obviously, not all procedures can work without lasers. Some, such as surgical soft and hard tissue removal, need a laser. Many procecures don't, however, and that's where consumer products come in.
My biggest lesson of WFLD is that it works. There's almost no topic in which you wouldn't benefit from light therapy. Thus, light therapy should be heavily promoted.
Items Mentioned In This Article
- Noovalab Novoral Care Pro - use discount code ALEX15 to save
- LightpathLED Diesel Torch - discount code ALEX saves
This is a post by Bart Wolbers of Light Therapy Insiders. Bart finished degrees in Physical Therapy (B), Philosophy (BA and MA), Philosophy of Science and Technology (MS - with distinction), and Clinical Health Science (MS), has had training in functional medicine, and is currently chief science writer.
Found This Interesting? Then You Might Like:
- Start Here - Light Therapy 101 & Buyers Guide
- Discount Codes, Deals & Recommendations - Red Light Therapy
- Red Light Therapy For Oral Health Ultimate Guide: 20 Unique Benefits!
- Oral Wound Healing With Red Light Therapy: Innovative Advancement?
- Dentin Hypersensitivity: Why Red Light Therapy Is A Game-Changer
- How Red Light Therapy In Dental Anesthesia Practices Shows Great Promise
- The Remarkable Role Of Light Therapy In Periodontal Care
- Dental Red Light Therapy Before And After Case Studies From Clinical Practice









