Let's talk about red light therapy for pancreatitis! This is a somewhat complex condition that's harder to diagnose for many people - and unfortunately, there's also not a ton of red light therapy research on this topic.
And yet, I'll make the best of it!
In this article, I'll help you understand the pancreatitis basics, some likely red light therapy benefits, and why you should always focus on lifestyle modifications, too. If you're short on time, then just read the summary below:
Red Light Therapy For Pancreatitis Summary
If you've got "pancreatitis" then your pancreas is inflamed. That organ is located in your stomach, a few inches below your chest. Different types of pancreatitis exist, such as acute and chronic, and there can be different causes for both.
Acute pancreatitis is often caused if you abuse alcohol or have gallstones, but, fortunately, also goes away quickly most of the time. Chronic pancreatitis is present for longer - as the name already implies - and also mostly caused by lifestyle factors, such as smoking and being overweight or obese.
Pancreatitis often gives symptoms that overlap with other health conditions affecting the stomach area, such as nausea, abdominal pain, poor digestion, etc. The pancreas is involved in both insulin function as well as digestion, so these symptoms aren't coincidental!
The diagnosis of pancreatitis often involves medical imaging, such as endoscopic ultrasound. To lower your risk of the condition, lifestyle modification is highly warranted - although doctors can keep you up with prescription medicine.
So, where does red light therapy come in? Some animal and foundational laboratory studies (in vitro) show lowered inflammation and enhanced pancreatic function with light therapy treatment. Human studies are sparse, but it's likely that many biological mechanisms, such as chronic inflammation, are affected by applying light.
More high-quality human studies are needed on this topic. But, if I had this condition, I would treat the area under my chest, around my lower ribs, with either handheld or tabletop devices, directly pressed against the skin for deepest penetration. Device suggestions are included in the full article! And, lifestyle modifications are essential if you've got acute pancreatitis multiple times or have the chronic variant!
Important Comments
If you need an introduction to what these terms mean, check the following resources:
- What Is Red Light Therapy?- Red Light Therapy Explained: Basic Terms Guide
- Start Here - Light Therapy 101 & Buyers Guide
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
- How Often Should You Use Red Light Therapy Explained
These resources should give you a basic understanding of how red light therapy works, and the discussions around it!
Understanding Pancreatitis
Let's talk about pancreatitis, which affects the pancreas. The pancreas is located below your liver, next to your stomach and spleen. As you can see in the picture below, these organs are located a few inches below the chest in your abdominal cavity:
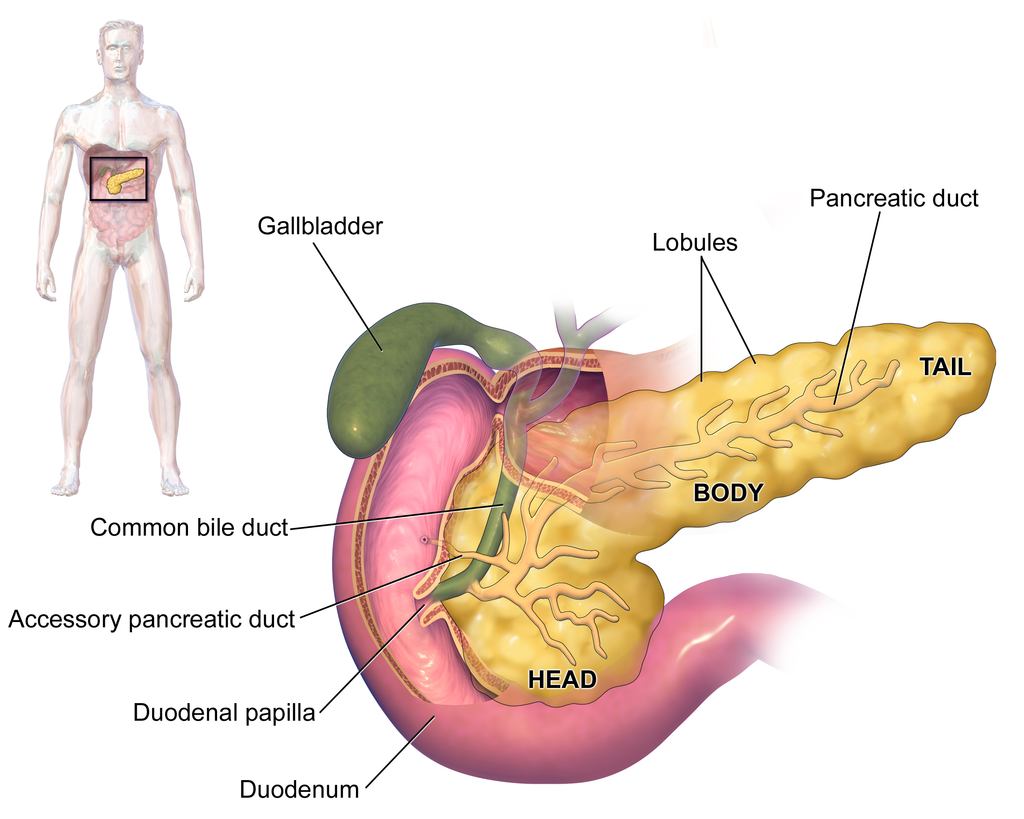
The pancreas is part of both your hormonal and digestive system - which shouldn't be surprising given its location (1; 2; 3; 4; 5)! The pancreas plays a part in your blood sugar management, hunger sensation, and aids digestion. The pancreatic juice helps neutralize acid in the first part of the small intestine after food has passed through the stomach.
The endocrine - or hormonal function - can be explained in the following way:
"The endocrine portion is arranged as discrete islets of Langerhans, which are composed of five different endocrine cell types (alpha, beta, delta, epsilon, and upsilon) secreting at least five hormones including glucagon, insulin, somatostatin, ghrelin, and pancreatic polypeptide, respectively." (1).
Glucagon and ghrelin are involved in hunger, among others! Somatostatin has a metabolic function, and insulin helps drive carbohydrates into your cells (although I'm oversimplifying). But with all organs, things can turn south. Type I and type II diabetes are two main instances in which there's often a problem with the pancreas (3; 4). In such cases, there are structural alterations to that organ.
Diet and lifestyle have a huge effect on pancreatic health in general for most (if not all) animals (6; 8). So if you're overweight or obese, pancreatic function tends to go down. What's interesting is that pancreatic transplantations often lead to huge improvements in health, such as in patients with type II diabetes (7). Other metabolic conditions besides diabetes and obesity can cause pancreatic issues as well, however (9).
You can also have pancreatitis - this article's main topic:
Pancreatitis: Different Subtypes
So, there are two basic types of pancreatitis, although it's more complicated than that - acute and chronic (10; 11; 12; 13; 14; 15). Pancreatitis is one of the leading gastrointestinal causes of hospital admission. As the name already implies, "pancreatitis" involves inflammation of the pancreas as an organ. As a result, pancreas function is inhibited, leading to a cascade of health problems down the road!
No bueno...
The acute type of pancreatitis often lasts a few days and emerges suddenly. Nevertheless, acute pancreatitis can still be dangerous and even life-threatening (12)! Chronic pancreatitis is present for a more extended period of time, and can even result in permanent damage to the pancreas if it persists (11)!
Hence, both types of pancreatitis need to be dealt with. And, if you're affected by one of these, I always recommend seeking medical support to avoid complications.
Now, both acute and chronic pancreatitis don't just spontaneously emerge, fortunately. You've got a great influence on the risk of getting either condition. There's a clear cause in 75 - 85% of all acute pancreatitis cases, which is either gallstone migration or alcohol abuse (16). For gallstones, the risk factors that you can modify are hypertension, excess body fat, thyroid problems (also often caused by unhealthy lifestyle), and diabetes (17).
Some acute pancreatitis can be caused by medication side effects, trauma to your belly, and infections.
Chronic pancreatitis signifies a pancreas that's inflamed over time. Here, eventually, the function of the pancreas is inhibited too. Chronic pancreatitis is primarily affected by your lifestyle once again as well (surprise, surprise!) (18; 19; 20). Smoking, being overweight, and drinking excess alcohol are important risk factors here. Having acute pancreatitis several times is also a risk factor for the chronic variant.
Generally, if you have pancreatitis, you'll know it. There's often nausea or vomiting, weight loss, swelling, pain in the abdomen, and the typical signs of disease such as a fever, rapid heart rate, and feeling unwell. With chronic pancreatitis, you can also have diabetes symptoms because digestion and metabolism aren't working properly anymore, and there are changes in your digestive capacity.
Treatment is also not without risk, but please consult your doctor for this topic. Doctors will diagnose pancreatitis with blood tests and imaging, such as endoscopic ultrasounds, MRIs, or similar, to distinguish the pancreatitis symptoms from other gastrointestinal problems. The issue here is that many symptoms of gastrointestinal problems overlap with pancreatitis, which is why you'll need specialized equipment for a medical diagnosis!
Your doctor and hospital know how to treat acute and chronic pancreatitis - so consult them on that topic! Overall, however, I strongly recommend fixing your overall lifestyle and nutrition to lower your risk of getting acute pancreatitis and potentially reversing your chronic status. Just avoiding smoking, cutting out excess alcohol (some is great and lowers mortality!), and getting to a healthy bodyweight are game-changers.
Yes, that's easier said than done, I know!
Next up, let's explore red light therapy and what it may do for you in this case:
Red Light Therapy, Its Benefits, And Its Effectiveness For Pancreatitis
I've written extensively about red light therapy in the past. Red light therapy uses both the red and the near-infrared part of the light spectrum that's emitted into your body. That red and near-infrared light penetrates your skin and then has biological effects in your body.
Light can be measured for their wavelength. Ultraviolet light - that can give you a sunburn - is found below 400 nanometers, for instance. And violet and blue light are found between 400 and 500 nanometers. Red light, moreover, is located between roughly 600 and 700 nanometers, and after that 700 nanometer range you've got near-infrared light, which is invisible to the human eye.
Different colors of light also have different biological effects. I'll mostly focus on red and near-infrared light here, however. So let's check out some of the benefits of red and near-infared light:
- Lowers inflammation
- Helps you lose fat and improves thyroid function
- Enhances gym performance and recovery
- Boosts hormonal function, such as lower stress hormones and higher testosterone
- Aids wound healing and makes your skin look more beautiful
- Helps brain function while lowering the risk of neurodegeneration
- Increase the amount of deep sleep you get
- Counters many types of acute and chronic pain, including joint pain
- Helps eye health, and counters many eye conditions
- Boosts your immune system functioning
- Lowers disease risk, such as heart and blood vessel condition, diabetes, and lung conditions, either directly or indirectly
- Enhances organ functioning
- Decreases stress and anxiety and helps well-being.
So that's great. If you want more extensive details, check my blog on the 36 powerful red light therapy benefits.
Next up:
How Red Light Therapy Penetrates Into the Cells
Like I've stated before in this article, the red and near-infrared light don't just touch your skin - that light penetrates into your body. In that body, they've got all types of different biological effects.
If you want a deep dive on this topic, check out my article on red light therapy and mitochondria. Red light therapy affects your body at the cellular level, by influencing energy production. Energy production is mainly affected through mitochondrial function. Mitochondria are the energy-producing factories of your cells. There, these mitochondria create "ATP" or "Adenosine-Triphosphate," which is considered the main currency of the cell - at least in conventional science, as smart people disagree there!
The overall functioning of cells increases by boosting energy-production and increasing mitochondrial efficiency. As a result, you'll move more towards health and away from disease. The simple truth is that energy is necessary for any cellular process to function, and with more energy, that process runs smoother. Red light therapy also has a strong effect on inflammation, reducing it, which is important in light of the topic of pancreatitis - an inflammatory condition!
Specifically, chronic inflammation is very strongly impeded by red light therapy. So, at least in theory, red light therapy should reduce your risk of chronic pancreatitis, although there's no direct research to be found on this topic as of right now.
Moving on:
Studies On Red Light Therapy For Pancreatitis
Unfortunately, there aren't too many studies on red light therapy for pancreatitis. There are a few specific studies on red light therapy and pancreas function in general, however.
Human Pancreatitis Studies
Here, I'll cover the 10 studies found in Vladimir Heiskanen's Excel sheet, including some studies on pancreatitis specifically. So let's go through all that research - at least the basics - and I'll tell you its significance in a moment:
- First, there's a study on pancreatitis and 630 nm light that's applied intravascularly, so inside your veins (21). Here, ceruloplasmin, which is involved in copper and iron metabolism, is normalized and may help promote countering pancreatitis, although much more research is needed. Study participants were treated 20 minutes per day for a week and their levels almost reached the same level as considered normal!
- Secondly, there's another study on participants with chronic pancreatitis, where the intervention group receives light therapy and the control group didn't (22). Researchers write:
" A total of 78 patients aged from 36 to 77 years were treated with [red light therapy] in addition to conventional therapy; the patients of the control group (n = 40) received only medicamentous therapy. Examination of the patients in the exacerbation phase of chronic pancreatitis revealed activation of [Lipi processes and differently-directed shifts of AOP components. These changes are supposed to reflect variations in the activity of the inflammatory processes in the pancreas and oxidative stress on this organ." (22).
- "Lipid peroxidation", as a process, is linked to pancreatitis, as it contributes to oxidative stress and cell damage in the pancreas - and is also linked to chronic inflammation! Unfortunately, the study shows few specifics of the treatment protocol so I can't learn any suitable lessons from it, except that the light therapy does work to lower some of the underlying biological mechanisms of pancreatitis!
- These are the studies on pancreatitis in humans - only two studies are available right now. Moving on to the next topic:
Animal And In Vitro (Laboratory) Pancreatitis Studies
So let's look at the remaining 8 studies, which are animal studies and/or in vitro (laboratory studies - remember science class as a teenager, such as petri dish studies) options:
- First, there's an 808 nm study with diabetic rats (23). The total dose was 30 J/cm2, although that dosing pattern differs for humans and animals. The rats retained body weight better and had a higher weight in the beta cells of their pancreas. These beta cells are involved in insulin creation.
- Then there's a 670 nm rat study where the effect was measured on the "islets" or "islets of Langerhans" - responsible for hormone creation in different conditions (24). A 2.8 mW/cm2 power output was used for seconds at the minimum and up to several days of dosing. Here's the quite positive outcome:
"In summary, for the first time, long-term [red light therapy] exhibited safety in terms of cell viability, insulin secretion, energetic profiles in vitro, and post-transplantation period in vivo. Further investigation is warranted to explore [red light therapy]'s protective effects under conditions of stress, aiding in the development of innovative approaches for cellular therapy." (24)
- A very recent in vitro study shows that light therapy promotes pancreatic cell viability in lab cultures (25). The results are promising under oxidative stress, one of the circumstances under which pancreatitis develops.
- One more 633 nm red light in vitro study tested a 0, 15.6, and 31.3 J/cm2 dose in pork islet cells (26). The results were decent, as the light increased the insulin secretion by these cells but didn't improve the responsiveness to glucose. So there was only a partial benefit here.
- Then there's 810 nm at 9 J/cm2, also in vitro (27). Different types of cells within the pancreas respond to that light well.
- Next up, there's a 630 and 810 nm in vitro study, although the study is a bit unclear and mentions 830 nm (28). Nevertheless, here's the result:
"Irradiation of incubated islets with 830 nm low-level laser significantly increased insulin secretion after a glucose challenge test (P < .05). There was a significant increase in insulin secretion after irradiation with joules/cm(2) 630 nm energy density (P < .001)." (28).
- In type I diabetes, 633 nm has positive effects on the health of beta cells, which are responsible for insulin production as well as other hormones (29). The light seems to induce beta-cell regeneration even!
- Another mouse study with 805 nm light shows similar results (30). Here's the insane difference in outcome when measuring how the intervention group (treated with 805 nm light) and control group responded to carbohydrates:
"[The D]iabetic group treated with LED showed regeneration of islets and ducts (p = 0.001) on the pancreas. Intraperitoneal insulin tolerance test showed differences between the diabetic control and diabetic treated groups (p = 0.03). In diabetic control group, the hepatic glycogen content was 296% lower when compared with diabetic treated with LED. Furthermore, in the diabetic control group, the glycogen content of the gastrocnemius muscle was 706% smaller when compared with diabetic treated with LED. This study shows that LED was able to modify morphological and metabolic features and also altered carbohydrate metabolism on irradiated pancreas in experimental model of diabetes."
- So in both animal and in vitro studies, red light therapy seems to have beneficial effects for overall pancreatic function!
So, Are The Benefits Of Red Light Therapy For Pancreatitis Backed by Science?
Well, I'd love to answer a resounding "yes" here. But there are a few complications:
- First, animal studies don't always translate directly to the same outcomes in humans. So we need human studies here to confirm these results.
- Then, it's pretty hard to properly treat the pancreas with sufficient intensities of light, as you'll need to penerate the skin and the light needs to venture inches into the abdominal cavity to reach the pancreas.
- Yes, dosing methods such as intravenous red light therapy may help here, but that's not an excellent option for the average person as it complicates treatment even further!
- Ideally, you'd have some human studies that use higher-powered lasers or even LED devices pressed directly against the skin at the height of the pancreas, with the observation of outcomes there.
- If you want to experiment yourself - which is 100% at your own risk and not medical advice - I'd personally use a handheld red light therapy device or a tabletop device under my chest, pressed directly against the skin. The area you'd want to treat is between around 2 inches above your belly button, and 2 inches below your nipple. For device recommendations, you may want to check the videos below.
- You may also want to treat the same area from the sides and the back of your body, such as at the same height but then from the sides and back. Here the light will have to penetrate the ribs, however.
For device recommendations, check:
And:
These devices should be big enough for spot treatment of the pancreas area. But again, we need more human studies to investigate how significant the effect will be when you're treating the pancreas through the skin with an LED device!
So that's my caveat!
Lastly, for this section, I'll leave you with one more suggestion:is the HEAL+ by Kineon that's specifically designed for the abdominal area - check Alex's review with the prominent science guru of Kineon below:
The Importance Of Lifestyle Modifications
The bottom line is, as always, that I recommend you fix your lifestyle and nutrition! Yes, it's easier said than done, and most people don't want to focus on these domains because it's harder than just doing some light therapy or taking a pill. Nevertheless, given the risk factors, I recommend:
- Stop smoking cigarettes if you do.
- Use moderate alcohol consumption - probably 2 glasses for men and 1 glass for women per day. I actually think moderate drinking is healthy, so there's no need to quit completely!
- Lose excess body fat.
- Lower your general inflammation levels - remember that chronic inflammation is linked not just to pancreatitis but to many chronic health conditions, such as heart disease, diabetes, neurodegenerative disease, organ problems such as fatty liver and chronic kidney disease, and more. There's no easy answer here, except for fixing your sleep quality, moving and exercising, eating healthy, etc! And, yes red light therapy for inflammation is a game-changer!
So that's it. The most important recommendations here. With the current evidence levels, light therapy only comes in much lower on that list. Until you and I can access much more high-quality human research, I can't strongly recommend light therapy. Nevertheless, I will say that the in vitro and animal research above is promising!
So there's that...
Conclusion: What’s Next For Pancreatitis?
Yes, unlike some other topics, such as red light therapy for autoimmune disease or red light therapy for rheumatoid arthritis, I don't have an easy answer here! With more human studies on red light therapy for pancreatitis, you'll likely get a much better picture of the influence of light therapy in the coming years or decades!
Nevertheless, I'm very hopeful!
Why?
Simple: the animal studies out there already are quite promising. And, often but not always, these animal studies translate into decent outcomes in humans as well. Then there's the fact that red light therapy positively affects many of the factors involved in pancreatitis, such as inflammation, poor digestion, and abdominal pain.
So, the future is likely bright!
This is a post by Bart Wolbers. Bart finished degrees in Physical Therapy (B), Philosophy (BA and MA), Philosophy of Science and Technology (MS - with distinction), and Clinical Health Science (MS), has had training in functional medicine, and is currently chief science writer at Lighttherapyinsiders.com
Found This Interesting? Then You Might Like:
- Start Here - Light Therapy 101 & Buyers Guide
- What Is Red Light Therapy?
- Discount Codes, Deals & Recommendations - Red Light Therapy
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
- Red Light Therapy for Arthritis: The Complete Guide
- 36 Powerful Red Light Therapy Benefits
- James Carroll Photobiomodulation Course: 16 Amazing Lessons Learnt









