In this blog post, I'll cover red light therapy for teeth and gums and other adjacent tissues. Many people tell me:
"But I've never seen a dentist use red light therapy in my life!"
"I don't know how to use red light therapy for gum and dental issues at my home?"
"There's no evidence that light even works for dentistry, it's all a placebo effect!"
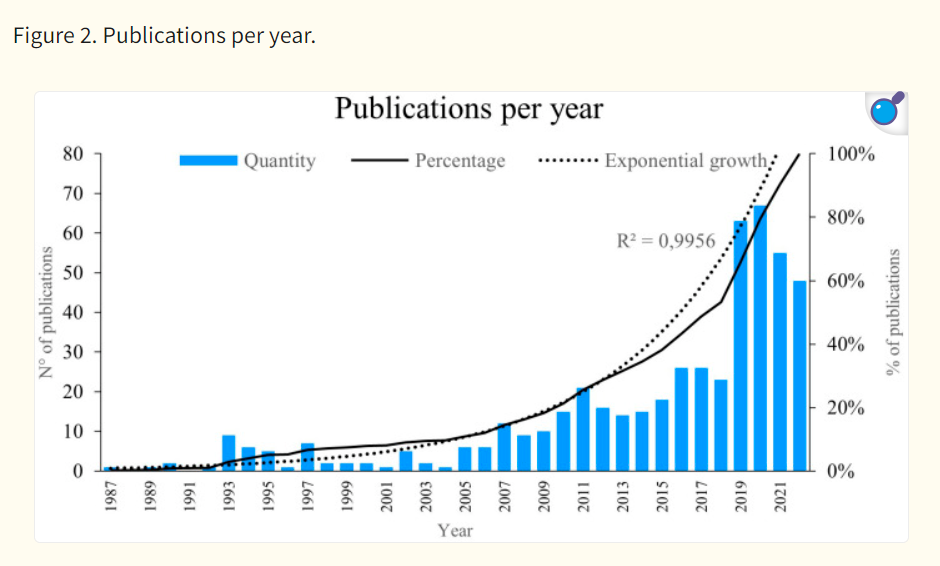
I'll deal with all of these statements in great detail one by one. But let me just say that there's massive evidence that red light therapy for dentistry works. How well it works depends on the goal you're trying to achieve, but right now, there are 1,800-2,000 different studies on the topic. So it's hardly an uninvestigated topic, especially given that red light therapy is extremely supportive across the board for oral health. You'll see in a second why I conclude that.
In dentistry and oral health, red light therapy has been proven to have many benefits. These benefits include pain relief, quicker tissue healing, lower inflammation and oxidative stress, and increased success in dental procedures such as orthodontics and endodontics.
Below I show 20 different benefits of red light therapy in dentistry. These include everything from reducing the side effects of teeth whitening procedures, to impeding anesthesia injection pain, to reducing the risk of side effects of cancer treatments, improving periodontal health, and lowering dentin hypersensitivity.
Red light therapy works through improving energy production while lowering inflammation. The exact mechanisms here, however, are in dispute and new additional mechanisms have been proposed. Nevertheless, with light exposure, the healing process improves and tissues in the oral cavity generally get healthier.
For each goal of light therapy for oral health, I've included specific treatment parameters such as wavelengths and the total dose (in J/cm2) if these are available. I've also recommended some devices at the end of this blog post. Sometimes it's difficult to give great treatment parameters, however, because studies differ so much from each other and there's no "one protocol to rule them all" - so to speak! In many cases, however, for each of the benefits I've covered below, more research is needed. Nevertheless, early results are extremely promising!
The good thing is, the research on this topic is growing (almost) exponentially. In my opinion, the effects or red light therapy can be life-changing for oral health! Those life-changing results are also the reason research is exploding in this area. And with that explosion of knowledge in the coming years, you can expect even better results in the near future!
My Methodology For This Article
As often is the case, I've used Vladimir Heiskanen's excellent datasheet that categorizes all red light therapy studies for my approach. And because this article is supposed to be an overview, I've restricted myself to the "systematic reviews" on each topic. Systematic reviews aggregate and analyze earlier research on a given topic.
So, if there are 20 studies on red light therapy for tooth extraction, the review analyzes these studies and gives you an overall picture of the topic. I had to limit myself due to the availability of almost 2,000 studies.
However, I try to give a comprehensive overview of red light therapy for oral health. So whether it's the effect of light on the nerves in the jaw, teeth whitening, orthodontics, or jaw problems, I've included all these topics in this article. For each topic, I'll consider the top 3-5 most recently published reviews and give you the most important lessons. So I'll pick the top 3-5 review on dental implants and red light therapy, 3-5 review on tooth extraction, and so forth.
I've broken all these topics down into 20 different benefits of red light therapy for dentistry. These benefits include anything for implants to oral surgery to periodontal health.
- Dentin Hypersensitivity: Why Red Light Therapy Is A Game-Changer
- How Red Light Therapy In Dental Anesthesia Practices Shows Great Promise
- The Remarkable Role Of Light Therapy In Periodontal Care
- Dental Red Light Therapy Before And After Case Studies From Clinical Practice
- Oral Wound Healing With Red Light Therapy: Innovative Advancement?
I'll summarize these articles below but for the scientific references, I'll refer to the articles themselves as I've spent tons of hours on each to make them awesome.
Understanding Red Light Therapy For Oral Health: The Basics
I've extensively talked about how red light therapy works in the past. The best article to read on this topic is that of red light therapy and mitochondria. There I explain that red light therapy enhances mitochondrial function - among other things. Mitochondria are the energy-producing powerhouses of your cells–but also have a role in immune function.
Mitochondria And Red Light Therapy
It's a bit oversimplified, but if your body isn't in an overstressed state, the mitochondria produce high energy levels. With age, mitochondrial function decreases because the DNA inside the mitochondria (different from your cells' center or "nucleus") diverges throughout the body. The end result is different diseases of aging, whether type II diabetes, neurodegeneration, heart disease, or other.
Red light therapy, fortunately, can increase energy production in the cell. The standardly accepted explanation here is that red light stimulates the last step of energy-creation in the cell, "cytochrome-c oxidase". Red and near-infrared light also likely stimulates the structure of water in the cell, as well as other mechanisms, through which the cell becomes healthier and increases energy production.
Energy is necessary for any process to occur in the cell to begin with. Without energy production, you would be dead. And with more energy production, you become healthier and more youthful. Inflammation and oxidative stress, which are intertwined with many chronic diseases, are lowered with red light therapy. Nevertheless, other factors, such as sleep, exercise, and a healthy diet, are crucial as well for optimal health so I don't recommend blindingly focusing on red light therapy only.
Red Light Therapy, Mitochondria, And Dentistry - The Basics
For oral health, red light therapy turns out to be really promising as well, through the mechanisms mentioned above. These mechanisms of lower inflammation and oxidative stress, and improving energy production, are intertwined. Let's explore the basics of those benefits below, where I consider red light therapy for dentistry in general first - before moving on to specific benefits.
If you wish to follow a great discussion on this topic, check out the interview with Prof. Dr. Michael Hamblin below - which also tells you that there's a lot in this field we still don't know:
If you need an introduction into what these terms means, check the following resources:
- What Is Red Light Therapy?
- Red Light Therapy Explained: Basic Terms Guide
- Start Here - Light Therapy 101 & Buyers Guide
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
- How Often Should You Use Red Light Therapy Explained
These resources should give you a basic understanding of how red light therapy works, and the discussions around it!
Red Light Therapy As A Breakthrough In Dental Care
So, red light therapy in dental care is really a breakthrough. Going through all these studies, I was really impressed by how groundbreaking light therapy is in many cases.
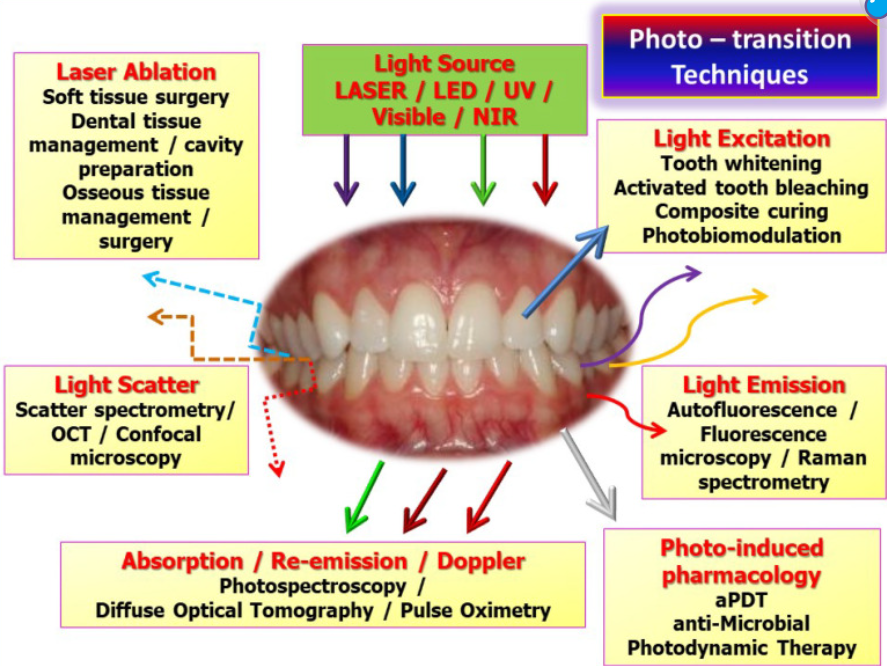
There is still discussion in the field about whether lasers or LEDs are equally effective, or whether one works better than the other (1). Light therapy has a huge range of applications, not only for your mouth and gums but also for interacting with medicine that may be used in your mouth (so-called "Photo Dynamic Therapy" or "PDT"), and for interacting with created biomaterials that are later placed in the mouth (2).
Light can also be as simple as applying blue light after you get a ceramic filling in your tooth. The blue light hardens the adhesive holding the filling in place (2). Many other processes exist here as well that I won't go into.
The amount of research on red light therapy for dentistry is exploding (3) A recent 2023 review writes that (3):
"The findings of this study demostrate that the scientific production related to [red light therapy] adheres to a growth power law, exhibiting characteristics of both exponential and linear phases. Notably, recent research trends emphasize critical concepts such as laser therapy, orthodontics, and dental pulp stem cells. Particularly significant is the burgeoning interest in utilizing PBM within dentistry as a complementary alternative to existing protocols."
You can see that almost exponential growth - exemplified by the "power law" above - here (4):
Interestingly enough, you can also see that the USA and Brazil are currently leading in the number of publications on this topic (4):
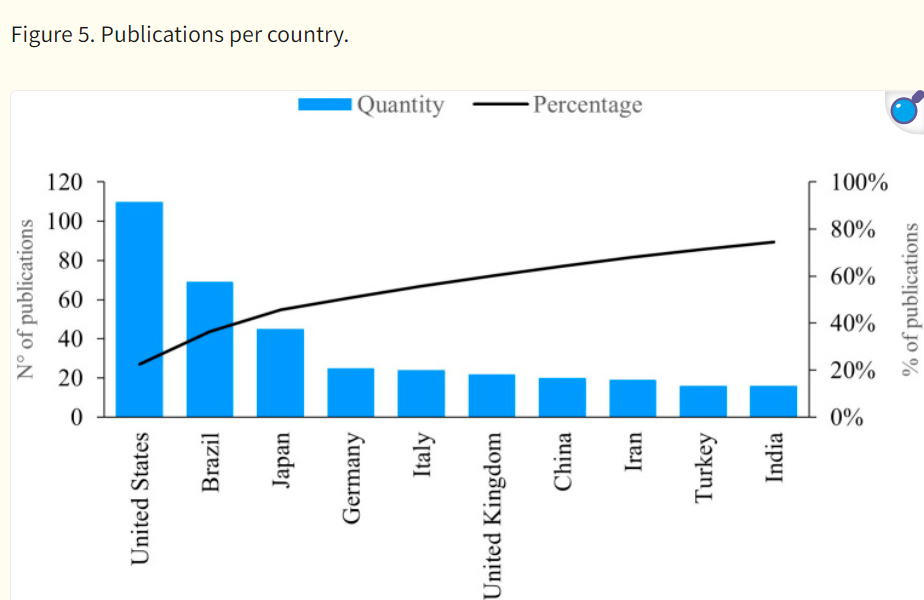
(I'm going to a laser dentistry event in Sao Paolo soon and will report on that on this website! Hence, my preparation of this article so I'm aware of the topics - I'm not a dentist but a health scientist myself.!)
The trend is fascinating as the developing world is now playing an active role in light therapy. I'm living in South America, by choice, and I've met some researchers from this region.
But let's go back to light therapy and dentistry. Pain is one of the most frequent reasons people visit a dentist. And (the fear of) pain is one of the most frequent reasons people don't visit a dentist. Pain, is a prime example of how light therapy can help people in this field (5). I'll venture into that topic in much more detail later on.
Overall though, the problem in the field is that treatment characteristics are often lacking - also in the light therapy and dentistry field (5). So, studies may not mention the size of the area that's treated, or the total dose in J/cm2, or the power output in mW/cm2. I've discussed this topic of missing information in research in detail in my PBM 2024 review article.
So, even though there's a lot of research in this field, Even though there's a lot of research in this field, there's a lot more work to be done. Studies need more rigor to develop standardized protocols.
Recent reviews mention that light therapy has widespread applications in dentistry (6; 7). Researchers write:
"In many dental specialties, [red light therapy] is a useful adjunctive treatment. On the hard and soft tissues of the oral cavity, it has a positive effect with fewer side effects." (7).
The complexity of dosing is an issue here, as are wavelengths used. The following picture shows that really well (8):
Unfortunately, I cannot give you a simple answer in this field, such as "use device X for Y minutes at location Z in manner A," because it would be an oversimplification. Read my article on red light therapy dosing to learn why.
I do add dosing guidelines at the end of this article. Those dosing guidelines allow you to reconstruct the dosing used in the studies, or at least approximate them, but you'd have to do some thinking yourself!
Dentistry is a complex field. Light therapy is a complex field. And their interaction is even more complex. I'll stick to the treatment parameters that are reported in the studies I'm quoting as much as possible and base my recommendations on those (8). These recommendations, then, yield the best evidence-based treatment parameters for different goals in dentistry.
Let's start:
20 Red Light Therapy Benefits For Teeth, Gums, And Other Tissues
Here I'll consider the most important topics that have been categorized by Vladimir Heiskanen in his red light therapy database on oral health one by one:
Benefit 1: Improves Analgesia And Lowers Anesthetics Injection Pain
Pre-treatment of an area that receives an anesthetic injection by the dentist with a laser for 1-2 minutes max lowers injection pain significantly. A 20-70 J/cm2 and near-infrared yield the best results. Pain levels, measured with VAS scales, go down by 20 - 40%.
So, "analgesia" (painkilling) and the injection pain of anesthetics are the first on my list. Here, you're using a red light therapy product to lower your pain levels. And, you're using a red light therapy product - almost always a laser in the dentistry office - to irradiate the spot where anesthesia is given with a needle.
Fortunately, I've already written a deep dive article on this topic: How Red Light Therapy In Dental Anesthesia Practices Shows Great Promise. So I'll summarize my findings below:
Red light therapy works wonderfully in conjunction with anesthesia. The light can be applied to the location where the injection needle is applied. As a result, the total amount of pain patients experience will go down by 20 - 40%, as measured on a "VAS" (Visual Analogue Scale).
The VAS scale measures pain from 0 - 100, where "0" stands for "no pain" and "100" stands for "the worst pain imaginable". So if you're at a 50-point VAS scale to begin with, which is moderate pain, your levels are lowered to a 20-point level, on average, which is almost no pain.
If red light therapy is applied before an injection, children's heart rates are lower, which signifies lower levels of stress. All these results can often be achieved by just a 1-2 minute treatment at the maximum, and far less if you have a high-powered laser as a dentist!
So why does this topic matter?
Well, as stated in the previous section, pain is one of the most frequent reasons people fear going to the dentist. Also, pain is one of the most frequent reasons why people skip the dentist for years - often making their problems far worse in the long run. Just the sight of needles frightens may people–and it's precisely the needle that is necessary in many cases to minimize pain close to zero!
Dentists already use anesthetic gels to lower the pain of needle injections. But adding red light therapy to that treatment often gives better results, or replacing the anesthetic gel with light therapy in the first place.
A dose of 20-70 J/cm2 needs to be used for the best results. That dose is likely inhibitory, especially for the more superficial skin tissues. Near-infrared light in the 800 - 900 nm wavelength range also has better evidence than red light.
There's less evidence that red light therapy has good effects on the duration of the anesthesia or its success. So right now, red light therapy is best used before anesthetic injections. And, because a dentist has to give that injection and you as a patient in 99.99% of cases don't know how that needle is placed precisely, at-home dosing of red light therapy is very difficult in this case.
Nevertheless, if you want more info, read my full article How Red Light Therapy In Dental Anesthesia Practices Shows Great Promise! Overall, near-infrared light is extremely promising for lowering injection pain and applications can already be considered a game-changer - especially for kids!
Benefit 2: Lowers Aphthous Stomatitis Pain And Boosts Healing
For aphthous stomatitis, there's a very strong effect on pain as measured with the VAS scale immediately, with 30 - 60% decreases, that continues up to one day after treatment. Healing time is also cut short. Use a dose under 12 J/cm2. There's no specific wavelength recommended.
Aphthous stomatitis affects your "oral mucosa". The oral mucosa is the "wet" inner part of the mouth. That mucosa plays a role in immune defence, among others, as well as breaking down food, and sensation. The mucosa starts at the inner part of your lips (that's not exposed to air if you've got your mouth closed) and includes the inner cheeks, the front part of the tongue, and the upper palate. What's crazy is that up to 20% of the human population is affected by this condition, according to a recent review (10).
With Aphthous stomatitis, that oral mucosa is inflamed (9; 10; 11; 12). You'll get small ulcers in the mucosa and discoloration (10).
Genetics play a role in the disease (9). Fortunately, there are several factors you can control with this disease, such as trauma to the location, psychological stress, your overall nutritional status (especially in relation to iron in the body, gut and digestive problems, and anemia (9). Quitting smoking also predisposes you to this condition somehow (9).
The regular course of treatment is prescription medicine in the form of corticosteroids (9). Anti-inflammatory drugs and antibiotics are also often used to counter Aphthous stomatitis (10). In more severe cases, systemic drugs are used instead of locally targeted drugs (10). Interestingly enough, a recent review states that lasers specifically need to be taken into account for treatment (11).
Chronic oxidative stress and inflammation play a significant role in this disease (12). Fortunately, that's precisely where red light therapy comes in. Two reviews show very positive effects of red light therapy for Aphthous stomatitis (13; 14). Here are the basics:
- The first 2024 review includes only randomized controlled trials (RCTs) - studies with an intervention and a placebo group (13; 15). A total of 14 previous RCTs were included here. The studies have many different wavelengths, such as 645, 660, 670, 809, 810, 940, 1,064, 2,780, and a few with 10,600 nm. Some of the studies don't even show the total dosage in J/cm2. Some of the lasers are pulsed while others are continuous. Then, the exposure time, the Wattage of the laser (which determines the power output to a large extent), and the treatment time all differ. So there's no universal protocol for Aphthous stomatitis right nowintense with red light therapy. Often, the laser treatment is not compared to a true placebo but against a topical treatment, for instance. When I look at the VAS scores, however, it seems that pain is dramatically reduced. Sometimes there's intense pain at the outset that's completely gone after one day. Some studies show a decrease of the VAS from a 4-5 or 8 to almost 0 (15). Another study shows a decrease from an 85 VAS (0-100) to 56 VAS immediately, and 31.5 the next day. Healing time is also significantly quicker than with placebo, with a mean difference of 2.55 days quicker healing time (15). You may need to apply the light regularly over time, however, at a moderate dose for the skin because these have an inhibitory effect. Doses used in studies range from 3 - 12 J/cm2.
- The second review has a similar conclusion but is from 2020 and doesn't take take the newest evidence into account (14).
Moving on:
Benefit 3: Counters Teeth Bleaching Procedure Damage (Teeth Whitening)
Red light therapy works in reducing hypersensitivity after the procedure. Bleaching procedures aren't benign, however, and may damage teeth. Near-infrared light (800 - 900 nm) has a slightly better evidence base than red light, and the best total dosages range from 4 - 20 J/cm2.
Yes, yes, I know. Everyone wants to look great! And for that reason, bleaching your teeth (or "dental whitening") is extremely popular in modern society. The procedure isn't without risk, however (16; 17; 18; 19; 20).
First, the process isn't forever, so you'll have to repeat the bleaching process every 1 - 2.5 years, regardless of the bleaching agent used (16). More importantly though, the pulp inside the tooth, that's located under the enamel (outer layer) and dentin (below the outer layer) is damaged by this bleaching process (17). Here's what a recent review concludes about this process:
"High-concentrations of bleaching gel increases inflammatory response and necrosis in the pulp tissue at short periods after bleaching, mainly in rat molars and in human incisors, in addition to greater hard tissue deposition over time" (17)
A total of 5/11 studies show inflammation of the pulp (17). This process can be so extensive that the entire tooth is damaged and root resorption occurs in the tooth - whereby it's destroyed from the inside out (20). In that case, the immune system cleans up the damaged tooth, and the tooth is gone!
There may also be irregular dentin dispositions - these often occur after severe damage (17). The result is often tooth sensitivity (18). Other problems occurring after bleaching are issues with the gums and damage to the enamel (18).
So both the teeth and periodontal structures can be negatively affected! Fortunately, some developments have made these products less damaging (19).
Those are the oversimplified basics. Now onto red light therapy. Two different reviews show that red light therapy does reduce hypersensitivity of the teeth after bleaching (21; 22).
The first review included six studies on this subject (21). And the second one included five studies on the subject (22). Unfortunately, I can't access the full text of these studies.
But, I can see the study details from Heiskanen's datasheet. The wavelengths here are mostly in the 600s and 800s, with some 900s studies and one blue light study. Near-infrared light is used lightly more than red light. Total doses range from 4 - 100 J/cm2, but the most successful studies stay under 20 J/cm2.
Benefit 4: Enhances Oral Bone Repair
Almost all studies on red light therapy for bone repair are positive and show quicker bone healing, less inflammation and less pain. A universal protocol is hard because studies diverge from each other. Nevertheless, the near-infrared wavelengths in the 800 - 900s range and power outputs up to 70 J/cm2 currently have the best evidence.
You may think: "What does bone repair have to do with my teeth? "
"Don't I have functioning teeth from my adolescence?
"And, almost nobody ever breaks a bone in their jaw, so why worry about this topic?!"
Well, it's not that easy! Your teeth themselves are bony structure and can be damaged over time (as you're well aware). So, the health of the teeth isn't given for anyone! These teeth are also tightly connected to the bone structure of the jaw. That jaw and its structure is extremely essential for proper structure of the teeth, especially in time when you get older.
My dentist friend Dr. Ana Paula Tanko has explained why in the article about clinical dentistry cases related to light therapy. Simply put, your jaw is the foundation of your teeth. Just like a house will become unstable without a proper foundation, the same is true for teeth as well.
If your jawbones are affected, they no longer offer the proper foundation for teeth. So bone repair and structure are of massive import. Bone repair is also essential for procedures such as placing implants, tooth extractions, periodontal treatments, and bone grafts. Bone grafts are a surgical procedure that adds substance to your bone to improve its structure. And, in the case you get trauma to your jaw or teeth, bone repair also matters.
As my friend Dr. Ana Paula explained, if your jaw's structure is compromised, it can eventually lead to periodontal problems and even tooth loss. Hence, if there's an issue with the bone, that needs to be corrected. Orthodontics and tooth implants may not work in this case because of a poor underlying foundation. Also, if you've got severe periodontitis (loss of gum tissue around the tooth), stimulating bone repair can also avert tooth loss.
Overall, bone repair is a highly complex subject, especially because there are many new techniques available (23; 24; 25; 26; 27; 28; 29). Stem cells are an example here, as is the 3D printing of tissue (tissue engineering), and platelet-rich plasma (PRP) (24; 25; 29).
Light therapy is another extremely promising technique for promoting bone healing around the oral cavity and jaw (30; 31; 32). Here's what the first review states (30):
"Eighty-nine percent of the studies revealed positive effects on bone formation between the laser group and the control group. Only one article reported that light-emitting diode did not significantly enhance osteogenesis [(bone formation)]. Additionally, the present study shows that Gallium aluminum arsenide of near infrared (NIR) laser with continuous mode is the most commonly used form of [red light therapy]. The biostimulatory effects are dependent on several parameters, with wavelength and dose being more important than others. Based on this review, it is suggested that the NIR range and an appropriate dose of [red light therapy] could be used to increase the efficiency of stimulating bone healing and remodeling."
So, near-infrared seems generally more helpful than red light. I can reconstruct the dose from Heiskanen's Excel sheet, have a range of 3 - 70 J/cm2. The wavelengths are mostly located in the 800s range, with about 70% in the 810 and 830 nm range.
But we end, once again, with the following dreaded statement seen so many times before:
"However, standardization of treatment protocols is needed to clarify therapeutic strategies in dentistry." (30)
So, once again, there's no "one treatment protocol to rule them all".
The second review shows that 11 / 17 previous studies have positive effects (31). The effects ascribed to light therapy are:
- Quicker bone healing
- Less pain during that bone healing
- Anti-inflammatory effects
- Beter quality of life in relation to oral health.
Lastly, a third–a somewhat older review from 2017–states that light therapy is tested in many different circumstances (32). Among these are tooth extraction, "jaw expansion" (maxilla expansion), periodontal treatment, cysts in the upper jawbone, and the growth of new bone between two separated bones (32).
Having all these different goals makes it harder to create a universal protocol once again because no circumstance is the same. Nevertheless, the conclusion remains that red light therapy supports oral bone (re-)growth!
Benefit 5: Impedes Burning Mouth Syndrome
Both red and near-infrared light work for burning mouth syndrome - a painful side effect of cancer treatment. Light therapy dosages vary a lot as well, going from 1 - 70 J/cm2. Pain is reduced with light therapy while quality of life increases.
"Oral dysesthesia" or "burning mouth syndrome is an altered sensation of in the mouth as a side effect of cancer treatment (33; 34; 35; 36; 37; 38). If you've got side effects from chemotherapy, there's a 13.6% risk of developing burning mouth syndrome (37). The condition may also be underreported, however!
You qualify for burning mouth syndrome if you have pain in the oral or facial area, with burning or altered sensations in the mouth, daily for more than 2 hours a day and more than 3 months–with no identifiable cause (33).
In this case, the nerves affecting the oral and facial areas are affected (33). However, there may also be a psychological component (36). Anxiety and depression can increase your burning mouth syndrome risk.
Both pharmaceutical and non-pharmaceutical interventions exist here - examples of non-pharmaceutical options are cognitive therapy, acupuncture, and, you guessed it: laser therapy (34). Pharmaceuticals and compounds such as capsaicin (found in hot peppers!) have the strongest evidence base right now (35). But, pharmaceutical interventions tend to have side effects here.
People of older age and women are more at risk for developing burning mouth syndrome (33). Oral-health-related quality of life goes down with burning mouth syndrome (38).
Fortunately, a couple of reviews from the last few years on burning mouth syndrome are available (39; 40; 41; 42):
- The first review includes 9 different studies (39). Treatment parameters vary wildly again, with doses as low as 1 J/cm2 at different points, and as high as 70+J/cm2 (43). Lasers are used, and small areas are treated on a point-by-point basis. Treatments vary from one to five times weekly. Study participants are tracked anywhere from a few weeks to multiple months, for the outcome. The VAS pain scale was reduced by 1-4 points, generally, in the laser group. The laser groups outperformed the control groups, including pharmaceuticals. Interventions longer than 4 weeks seem to work slightly better here. Near-infrared above 700 nm works equally as well as red light. The quality of life improved, as did the number of negative emotions–although the effect here was small.
- A second review included 7 previous studies and found that red light therapy decreased pain more than other treatments (40). Light also improved the quality of life. Paradoxically, red light worked better in this study than near-infrared! But, the study is one year older and doesn't consider all the data. Nevertheless, I'd conclude here that red and near-infrared probably both work equally well. Quality of life also improved with red light.
- Two older reviews from 2021 do find positive effects but have minimal data (41; 42). This shows you how quickly this space is developing!
Benefit 6: Aids Dental Implants Acceptance In Tissue
Wavelengths between 600 - 1,1000 nm, with total dosages of 7 - 90 J/cm2, applied directly to the tissue of where a titanium implant is placed, improve implant stability and bone density near the implant.
Dental implants are a vital part of modern dentistry. And sure, most of the time, tooth loss or damage can be avoided by simply having a healthy lifestyle and proper oral hygiene practices, among others.
But it's not always up to you! In some cases, you may need a dental implant because of trauma. When I was in Turkey this March and April, I met a young British guy who got four of his incisors torn out after a road trip on Ibiza. Sheer bad luck, or was there more to the story? Anyway, the guy needed dental implants and went to Turkey to get them done.
If you're young and lucky, dental implants generally work well because of the quick bone and soft tissue healing you'll have at that age. The story gets more complicated when you're older and generally more prone to need dental implants. The healing process is typically slower, but the jaw structure may also be poorer at that age, making integrating the implant more difficult. Health conditions such as diabetes and lifestyle factors such as smoking further slow down the healing process (43).
Implants are a wonder of modern dentistry - the current form of implants that go directly into the bone has only been around for a few decades! Fortunately, implants currently have a 97% success rate (44). Improper implant integration into the bone is the biggest risk here (46). Bruxism or teeth grinding - which I also suffer from! - also increases the risk of implant failure (52).
The big benefits here are saving your overall dental health compared to when you would choose other options such as fixed partial dentures. Your jawbone's integrity stays stronger with implants compared to other options, adjacent teeth have less (hyper)sensitivity, and there's even a lower risk of caries in adjacent teeth (44).
Teeth are generally superior to implants, however (45). So keeping your own teeth should always be a priority. The longer-term success rate of dental implants is also lower and could lead to complications (47). I'm personally fan of ceramic implants because they are hypoallergenic and don't implant a conductive metal in your mouth that interacts with Electro-Magnetic Frequencies (EMFs). Most of dentistry uses titanium implants, however, which are less expensive.
But let's consider how red light therapy can help for dental implants. Here are the systematic reviews on this topic:
- A 2024 review shows that red light therapy improves bone density (48). Recall that integration of the implant into the jaw - called "osseointegration" - is the trickiest part of the process. Implant survival and bone loss during the process don't differ.
- Another 2024 review shows that implant stability improves with red light therapy applied (49).
- A 2023 review investigates treatment parameters very closely of 15 previous studies (50). Researchers state that:
"Laser and LED wavelengths that reported significant results included 618, 626, 830, 940 (2 × ), and 1064 nm." (50)
- The treatment area is almost always smaller than 1 cm2, except for one study (51). The total dose differs between 7 and 90 J/cm2, mostly. There are some exceptions with a 135 and even whopping 3,750 J/cm2 total dose - especially the latter I choose to ignore here. The latter study only treats a minute area, however, and still has a positive outcome!
- Treatment can occur with the contact method (51). So the 7 - 90 J/cm2 (and more if you only treat a minute spot) will help overall implant stability.
Benefit 7: Strongly Inhibits Dentin Hypersensitivity
Both red and near-infrared light are extremely helpful for dentin hypersensitivity, as a single treatment can often lower pain levels by 40 - 70% over the course of months. The recommended dosage here is 2 - 10 J/cm2. I advice you to get the LightpathLED Diesel Torch for this purpose, with the oral tip (discount code ALEX saves!)
I wrote a very extensive article about red light therapy for dentin hypersensitivity before. Check that article here: . I'll still give you a summary below though:
Dentin hypersensitivity is characterized by pain due to stimuli such as heat, cold, or pressure, affecting the dentin in your teeth. Dentin is the layer beneath the tooth's enamel - the hard outer part of your teeth. The microscopic tubules in the dentin that transmit sensory information trigger that pain.
Conventional treatments for dentin hypersensitivity include fluoride applications, specialized toothpastes, or numbing agents. These methods have limitations, because they have side effects and don't treat the root cause of the problem.
Dentin hypersensitivity is also underdiagnosed because most dentists don't inquire about it. The diagnosis of dentin hypersensitivity often relies on patient self-reporting.
Red light therapy has emerged as a promising alternative for dentin hypersensitivity. Many Randomized Controlled Trials (RCTs) have investigated its effects on dentin hypersensitivity. Remember that RCTs use a control group that gets a placebo treatment and an intervention group that receives the actual treatment.
The best wavelengths used in these RCT studies are the 630, 650 - 660, 808 - 810, and 1,074 nm light. Doses of 2 - 10 J/cm2 work best for hypersensitivity, applied directly to the affected tooth with a spot treatment device. I recommend the LightpathLED Diesel Torch here because it has an oral tip that allows you to treat individual teeth (discount code ALEX saves!).
You may either treat the tooth itself or the gum area around the tooth so that the cervical (middle) region of the tooth is treated or its root (lower part).
The light treatment listed above leads to big reductions in pain, often 40 - 70%, as measured on a VAS scale. The pain reduction also lasts several months in studies that measure it. No side effects are reported.
Red light therapy likely alleviates pain through several mechanisms: modulating neuronal function, reducing inflammation, stimulating blood flow, and encouraging tissue repair. These effects can lead to a deposition of secondary dentin, which decreases dentin permeability and pain over time.
Don't focus only on red light therapy, however, if you want to counter dentin hypersensitivity. Other strategies include good oral hygiene through the use of remineralizing toothpaste like those containing hydroxyapatite, healthy dietary habits, and lifestyle changes that reduce exposure to acidic foods. You'll also want to minimize abrasive brushing techniques.
Furthermore, my friend Dr Ana Paula Tanko mentions that 95% of cases of dentin hypersensitivity are caused by bruxism either during the day or at night. Being aware of bruxism during the day and wearing a mouthguard at night should fix most of these cases long term. Red light therapy should still be used to lower pain, however, and in case bruxism isn't the root cause of the problem.
Bruxism puts transversal pressure on the teeth, which affects the cervical (middle) area of the teeth the most. Of course, there's wear and tear on the top (enamel) surface of the teeth, but the midsection of teeth is also affected strongly. By fixing the bruxism, you will fix the root cause of the dentin hypersensitivity and it should disappear. You should wear a mouthguard at night for protection because you may unconsciously grind your teeth.
Again, if you want a deep dive on this topic, check my article: Dentin Hypersensitivity: Why Red Light Therapy Is A Game-Changer
Benefit 8: Improves Dry Mouth
A whopping 23% of the world's population is affected by dry mouth. A dry mouth is an inferior saliva production that has negative consequences for overall oral health.
Your best bet here is a combination of red and near-infrared at 2 - 10 J/cm2, applied to the outside of the mouth into the salivary glands. These glands are located in your cheeks and under your tongue. Use a handheld red light therapy device for this purpose.
A dry mouth is also called "xerostomia" or "hyposalivation." "Hypo, here, means "low" and "salivation" relates to the saliva production in your body. That saliva is of utmost importance for your overall oral health. For instance, (re-)mineralization of the enamel and dentin partially happens through the silva.
The saliva helps break down food and protects against harm such as acids (think citrus fruits!). The growth of harmful bacteria is limited by sufficient saliva. And sufficient saliva is also essential for speaking and swallowing. Just remember when you had a presentation, were stressed, and had a dry mouth as a result - pronunciation suffers in these circumstances!
Over time, a lack of saliva not only creates problems for the enamel but also the gums. Periodontal disease risk goes up, for instance, as does the risk of Candida infections.
The risk of dry mouth increases with age (53). A whopping 60% of older adults have dry mouth (53). And taking multiple medications is one of the main risk factors for developing dry mouth (53). Chronic health conditions, such as diabetes type II and heart and blood vessel disease, are other major risk factors (53). Here's a quote on the link between dry mouth and your overall health that's really frightening:
"An increase in the number of medicines taken, from 0 to 5, decreased the number of natural teeth remaining from 16 (standard deviation [SD] ± 9) to 12 (SD ± 8), respectively. Additionally, the number of dental complications increased from 1 (SD ± 2) to 2 (SD ± 2) as the number of medicines increased from 1 to ≥ 3. There was a paucity of studies (n = 2) that investigated psychological health conditions of dry mouth among older adults, with depression identified as a significant issue among older adults with dry mouth (where the reported prevalence was as high as 64%)." (53)
In plain English, there's a correlation between more prescription medication taken, dry mouth, and the loss of teeth. A higher intake of prescription medicine is also correlated to more dental complications. I know correlation isn't causation, but testing this hypothesis in an RCT study is completely unethical! Dry mouth is also linked to depression.
Now here's another scary statistic: 23% of the world is currently affected by dry mouth (54). So it's not only older adults that are affected here. Why? Taking three or more prescription medications increases your dry mouth risk by 2.9X (54). Antidepressants, such as TCA's or SSRI's may be especially responsible for this increase (55). Denture wearing also increases the dry mouth risk (56). Neck and head irradiation because of cancer treatment is another common dry mouth cause - as is smoking and alcohol use.
One solution to increase saliva production is to chew xylitol gum. Xylitol also stimulates good bacteria in your mouth. Then there's red light therapy as well! A few reviews have been written on this topic in the last few years:
- A 2024 review shows that stimulating the saliva glands in the cheeks helps cancer patients with dry mouth because of radiotherapy (57). This review singles out 630 and 830 nm as the most promising wavelengths, at 2 - 10 J/cm2, two to three times per week. Stimulating the area around the glands with LEDs instead of a very targeted approach seems to have the best effects. The light therapy is best used before and after radiotherapy. Pain goes down while salivary flow goes up.
- Another 2024 review also concludes that red light therapy for dry mouth is promising - this time in patients with neck and head radiotherapy (58). The review includes four earlier studies. Four studies use infrared light, and two of these include red light. Quality of life improved with red light therapy.
- A 2023 review shows that TENS ("Transcutaneous Electric Nerve Stimulation") may help even more than light therapy (59). I really suggest you try TENS out if you've got dry mouth, or one of your loved ones, as it's a hit or miss therapy whereby you'll immediately know whether it's working or not. I know TENS from my early days as a physical therapist in the 2009 - 2010 era!
- A 2022 study has more or less the same outcome as the earlier studies (60).
If you want to recreate this scenario, I'd recommend using a handheld red light therapy device that my friend Alex Fergus has reviewed here:
Check out our shopping tool as well - here you can select devices with 630 and 830 nm light.
Benefit 9: Enhances Endodontics Procedure Success
Red light therapy lowers postoperative pain after endodontic surgery. Pain is often a complication there, and wavelengths from 600 - 1,000 nm have an inhibitory effect. Power outputs that work vary wildly, ranging from 4 - 600 J/cm2. Treatment should be applied by a dentist specialized in red light therapy, however! Pain measurements may be cut in half with red light therapy.
Endodontics refers to the pulp inside your teeth and the surrounding tissues. Below the hard outer enamel layers and the dentin layer below that, there's the dental pulp. That dental pulp causes extreme shooting pain if you've ever had caries progress so far that the enamel and dentin layers were fully penetrated.
Endodontics aims to preserve natural teeth that have become damaged or infected (63; 64; 65; 66; 67). And by maintaining your natural teeth, you're retaining your oral health and, thereby, your overall health–at least, that's the thought behind it.
Why?
Well, the most common endodontic procedure is a root canal treatment. In a root canal treatment, inflamed or infected pulp is removed. The area is then cleaned and disinfected and subsequently filled and sealed. Filling and sealing prevent further damage, the theory goes.
Root canal procedures are highly controversial, however. Many holistic and biological dentists don't like them. An example here is Dr. Dominic Nischwitz, who has the following explanation:
Other dentists I regard very highly disagree and still carry root canal treatments out (61). Everyone agrees, however, that it's best to retain your regular teeth and avoid root canals in the first place. But that's easier said than done–especially if the damage was already done!
Endodontists aim to manage complex cases involving intricate root canal systems or persistent infections. Modern technology helps endodontists massively to do their job better due to better imaging, disinfection, and sealing of the root canal.
Whether you accept root canal treatments or not, the goal here is to promote long-term oral health. If you get a root canal, at least have it carried out by an experienced endodontist. Having a specialist carry out the job massively decreases your risk of long-term problems!
Simple!
Root canals can work but it's up to you whether you accept the risk tolerance (62). There's an about 70% success rate over 37 years. And if a root canal fails you, you can always get an implant anyway. Many of these root canal-treated teeth didn't even use the latest technologies that are used in 2024, so today's success rate would be far higher.
Four reviews exist on modern endodontic surgery - specifically postoperative pain (68; 69; 70; 71). I'll go through these reviews one by one:
- A 2024 review shows that 7 / 9 studies lower postoperative pain with red light therapy after endodontic surgery (68). Eight studies here show no adverse effect and only one showed downsides when the pulp was chronically inflamed in an irreversible way. All of these studies are RCTs (72). Wavelengths used are 660, 808, 780, 905, 970, and 980 nm. The total dose is 4 - 40 J/cm2 in the lowest studies, 85 J/cm2 in the middle range, and 320 and 600 J/cm2 at the higher end of the studies. Remember that for painkilling purposes, however, higher doses may work far better because they have an inhibitory effect. Treatment time was between 8 seconds and 3 minutes - so it's a cost-effective treatment!
- A second 2024 review also shows benefit of the 800 - 900 nm range, but is skeptical about the total dose applied (69). Nevertheless, most studies show a positive outcome for pain after endodontic surgery.
- A third review considers root canal re-treatments, so treating a root canal-treated tooth a second time due to arisen problems (70). Pain measurement scales such as the VAS I discussed or the NRS score about half in the light therapy treated groups (73)!
- The last 2021 review has the same conclusion as the ones above (71).
Some other reviews also consider red light therapy for endodontics in general. A 2023 review writes that:
"[Red light therapy] stands out in the realm of dentistry for its unique attributes that set it apart from traditional therapeutic approaches. This non-invasive and painless modality harnesses the power of low-intensity lasers, offering a distinct advantage in terms of safety and patient comfort. Unlike many conventional methods, [red light therapy] does not rely on pharmaceutical interventions or invasive procedures, making it a gentle yet effective option for various dental applications. Its non-thermal, photobiomodulatory effects on cellular and tissue functions mark a notable departure from the more aggressive treatment modalities commonly associated with dentistry." (74)
Another 2020 review also shows that 14 / 17 studies have positive outcomes for endodontics with lasers, with no side effects (75).
Benefit 10: Lowers Pain And Inflammation With Graft Versus Host Disease
Red light therapy is a great adjunct therapy for graft versus host disease (GVHD). GVHD happens when your immune cells attack the cells added to your body after a necessary stem cell transplant of cells that aren't your own. Pain and inflammation are reduced with red light therapy.
Graft Versus Host Disease (GVHD) is an immunological reaction that happens with transplants. Stem cells and donor tissue are the main culprits here. What happens is that your own body's immune cells attack the new tissue that is identified as "non-self" tissue by that immune system. This immune attack usually occurs with donated stem cells that aren't yours or with graft tissue (76; 77; 78; 79; 80; 81; 82).
In the oral cavity, GVHD can manifest as mucosal lesions, ulcers, and erythema, leading to pain, difficulty eating, and increased risk of infections. In time, GHVD can turn chronic. Chronic GVHD may cause fibrosis, salivary gland dysfunction, and xerostomia (the dry mouth I discussed before). These problems elevate the risk of dental caries, periodontal disease, and oral candidiasis.
The management of GHVD in dentistry typically includes meticulous oral hygiene, use of topical steroids, saliva substitutes, and antifungal treatments to alleviate symptoms and maintain oral health.
In the body in general, moreover, GHVD can result in damage to multiple organs, including the skin, liver, and gastrointestinal tract. GVHD is categorized into acute (occurring within the first 100 days post-transplant) and chronic (occurring later, with symptoms persisting for months or years). Oral manifestations are common in chronic GVHD, affecting up to 80% of patients.
In the worst-case scenario, chronic GVHD is associated with an elevated risk of developing oral cancers, particularly due to chronic inflammation and immune dysregulation. Dentists play a crucial role in managing oral GVHD. Regular dental visits help monitor for early signs of oral lesions or malignancy.
But why would you choose this stem cell intervention anyway? Why take this stem cell intervention with the risk involved?
This so-called "Allogeneic hematopoietic cell transplantation (allo-HCT)" is only used in extreme cases. In these cases, your bone marrow is diseased, and the donor stem cells can restore normal blood production. Or, there may be a case of cancer, and stem cells may be used as part of the cancer treatment. In both cases, there's no option to use your own stem cells–hence, another option is necessary!
Now let's consider the oral aspects of GVHD, especially red light therapy. There's only one good review here:
- A 2024 review shows that red light therapy is a great addition to the treatment of GVHD (83). Pain and inflammation are lowered. Function improves with red light therapy. Unfortuantely, I can't access the full text of this study so I can't get any dosing parameters. Also, with cancer, please consult with your dcotor first before applying redlight therapy.
Benefit 11: Curbs Lichen Planus Pain And Inflammation
Different wavelengths in the red and near-infrared light spectrum - from the 600s to 1,064 nm - work. The best total dose is likely located between 1.5 and 12 J/cm2.
Red light therapy works equally well as corticosteroid medication for pain and the clinical assessment when leasions are treated. Lichen Planus is an autoimmune disease that's explained in more detail below:
Lichen planus is an autoimmune disease that affects the soft tissues of your body (84; 85; 86; 87; 88). These tissues include the skin, hair, nails, and the mucous membrane in the mouth. As with most autoimmune diseases, lichen planus is characterized by inflammation.
With the mucous membrane in the oral cavity affected, you're getting white patterns on the cheeks, gums, tongue, and potentially lips (87). These white patterns can be paired with redness. Pain's also often involved with the inflammation, and if things get terrible, there's swelling and open sores.
Lichen Planus' cause isn't fully understood right now - as is true for most autoimmune diseases (85; 88)! Nevertheless, if your health goes south due to stress, trauma, or infections, for instance, the Lichen Planus can be triggered. Some prescription drugs can also trigger Lichen Planus (84).
Lichen Planus doesn't just give you pain, however. Due to the sores and inflammation, speaking, eating or swallowing can get more difficult. Also, you may tolerate spicy or acidic foods less well than normally (86). Generally, however, Lichen Planus can be managed well.
The solution to most Lichen Planus cases is to use prescription medication. Examples here are anti-inflammatory drugs or painkillers (also applied locally). You'll also do well to lower your stress levels and avoid anything that can trigger the Lichen Planus, such as alcohol or smoking. Fortunately, there's good news as well! A few recent review studies have been published on red light therapy for Lichen Planus that I will break down below (89; 90; 91):
- First up, a 2024 review included 8 previous studies (89). The main lesson scoreswas that red light therapy worked equally well as corticosteroid medication. So, you can use red light therapy if corticosteroids can't be usedor side effects that you want to avoid. Both pain and clinical scores scored equally well in these cases. Seven out of eight studies are RCTs here. The wavelengths used are 630, 660, 808/810, 970, and 980 nm (92). Totally applied dosages are 1.5 - 12 J/cm2 on the lower end, and 150 - 177 J/cm2 at the higher end (but treating small areas (92). Here's the explanation that is given as well:
"[One group of authors] have reported that [red light therapy] is a more effective intervention for the treatment of [oral lichen planus]. These findings are also supported by [two other author groups]. On the other hand, five other trials have reported that [red light therapy] is less effective than control interventions in improving pain scores. Hence, the pooled analysis could not specify the superiority of one treatment over the other. The variation in individual trial results might be attributed to different parameters that affect the treatment, including wavelength, power, energy density, treatment duration and intervention time, method of application, structure, and condition of the tissue" (92)
- The three studies that work best, here, seem to be studies with lower total dosages (92).
- Another 2024 review explores the same topic and includes ten previous studies (90). Here there was a benefit of red light therapy over corticosteroids for pain, when they were compared. Red light therapy had no reported side effects. However, more research is needed with bigger groups of participants. Nevertheless, a very exciting outcome!!
- A third 2022 review includes seven previous studies with wavelengths between 630 and 1,064 nm (91). Here the light therapy counters lichen planus lesions. Great stuff!
Benefit 12: Aids Oral Nerve Recovery, Pain, And More!
Light therapy can aid nerve recovery, especially in the longer run such as 30 days after an injury or post-surgery. Near-infrared wavelengths have the best profile right now, and dosages between 1.5 and 30 J/cm2 for the inferior alveolar nerve (the lower jaw). For the trigeminal nerve higher up the face, 808 nm at 12 J/cm2 seems to work best.
Due to the very divergent nature of the reasons nerves are affected, however, it's impossible to come up with a universal protocol. It's best to have a medical professional in dentistry who has experience apply red light therapy in this case.
Recovery rate, pain, sensibility, can all improve dramatically long term with red light therapy for nerve injuries. Treatment within a few months of the injury is important for the best results.
Well, the the topic of oral nerves is somewhat complicated because different nerves that are affected have wildly different effects (93; 94; 95; 96; 97). The trigeminal nerve, for instance, can give rise to pain that you wouldn't wish upon your worst enemy - I've seen patients with this problem during my physical therapy time 1.5 decade ago now!
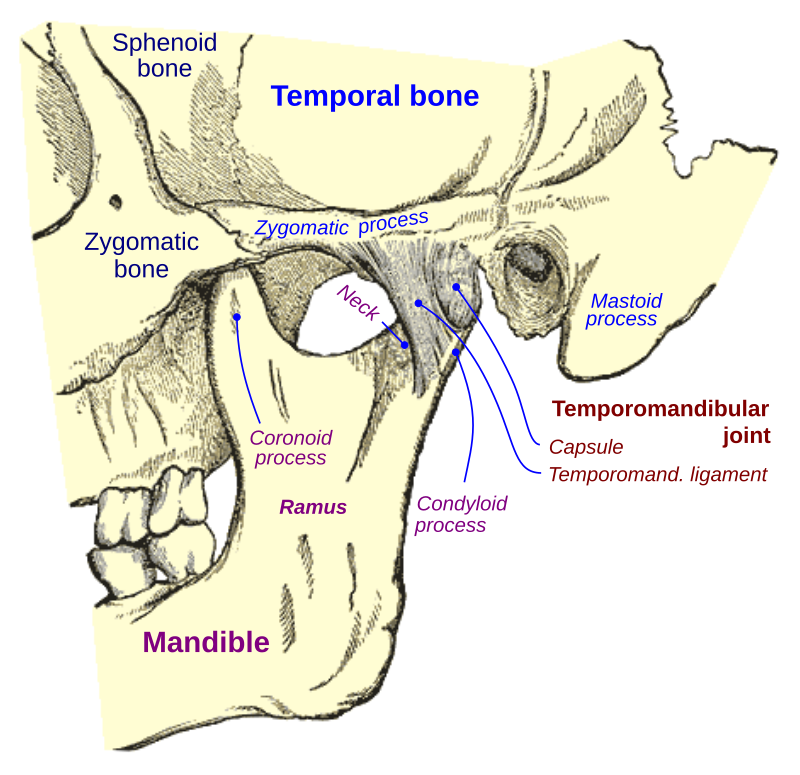
You can see the nerves originating from the jaw joint area in the picture below:
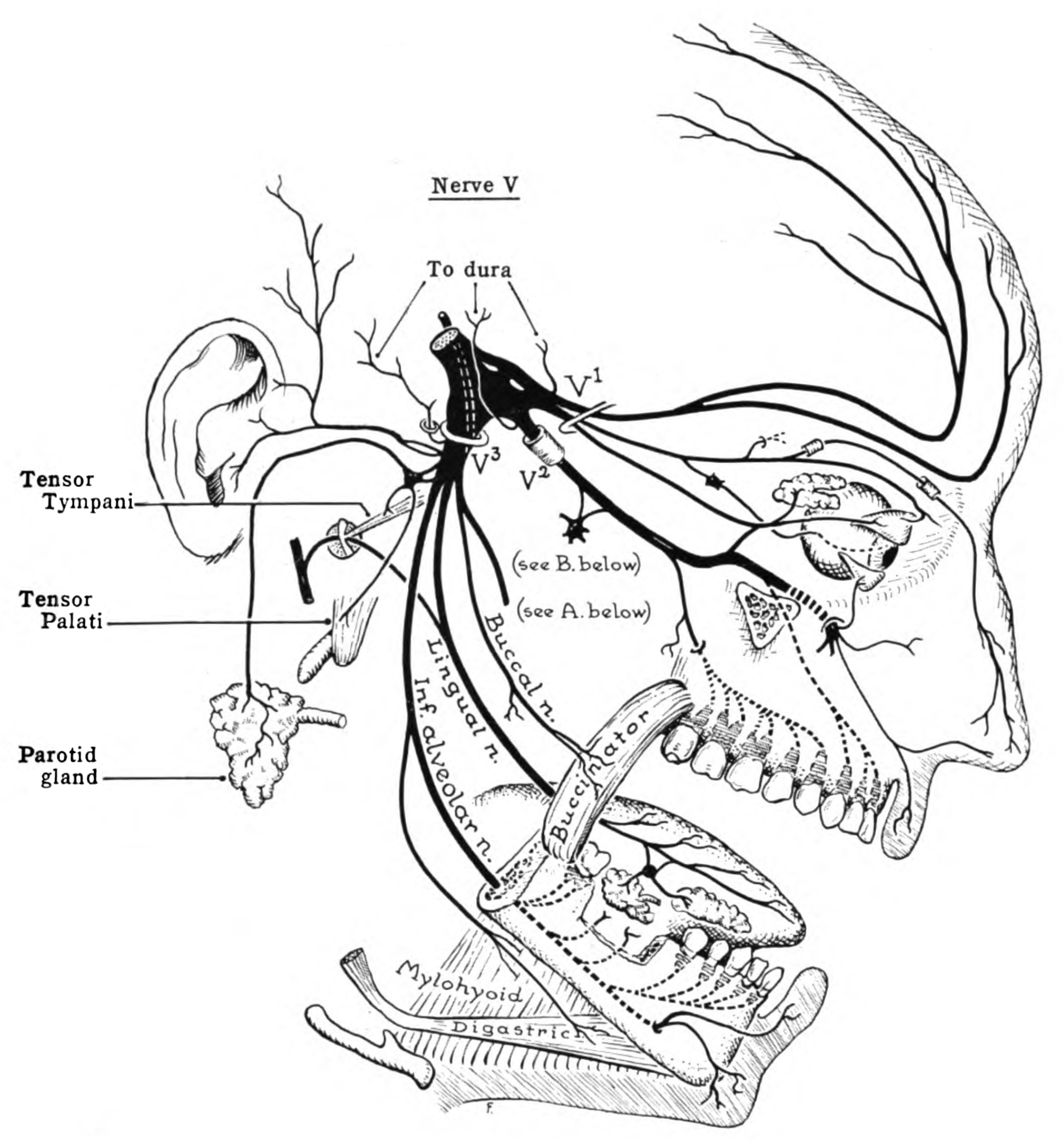
If you watch closely, the Buccal, Lingual, and inferior Alveolar nerve all originate from the same place: the trigeminal nerve. Here's a breakdown of the nerves in the lower jaw - the mandibular division of the trigeminal nerve:
- Buccal nerve: provides sensation in the cheek skin and the mucosa in the mouth.
- Inferior alveolar nerve: gives sensory input to the lower teeth and the mental nerve. The latter provides sensation in the chin and lower lip.
- Lingual: creates sensation in the front 2/3rds part of the tongue.
The mandibular nerves also supply motor function, meaning that they help move the jaw itself. Then there's the upper jaw - the maxillary division of the trigeminal nerve:
- Here there are four divisions and a few subdivisions that I won't go into. I hope you get the idea. Some parts supply sensation to the upper teeth and gums, others to the area under your eyes, others to parts of the cheek, and so forth!
Suffice it to say that the anatomy and functioning of these nerves in the jaw, cheeks, and oral cavity is complex! Many things can go wrong concerning these nerves. And, the nerve or the branch of a nerve that's affected determines the outcome for your oral and jaw health.
For instance, you can get a nerve injury after dental work. Examples here are root canals, or implants, and especially tooth extractions. If a nerve is damaged, you may end up with sensation loss in an area around your mouth or jaw. Or there may be pain or tingling.
Sometimes, dental procedures unintentionally damage a nerve, leading to neuropathic (nerve) pain. And tooth or jaw infections can also affect the nerves if they spread.
And, as stated before in this section, if the trigeminal nerve itself is affected, you can end up with "trigeminal nerve neuralgia" - one of the worst chronic pain conditions that change your life for the worse!
Next up, depending on the nerve affected, the jaw joint itself may be affected, leading to Temporomandibular joint (TMJ) disorders - a topic I've considered in an independent section below! Jaw problems can lead to headaches, having a harder time chewing, or facial pain.
Fortunately, there are some reviews on red light therapy for oral nerve injuries (98; 99; 100; 101)
- A 2023 review shows that red light therapy had no effect in a period of 14 days or less but did after a month for the inferior alveolar injury (98). For thermal discrimination, there seems to be less of an effect. The inferior alveolar nerve gives sensation to your lower teeth and chin. The review included 14 previous studies. Wavelengths differed between 780 and 980 nm for lasers, and an LED study used 632 and 850 nm (102). The total dose differed between 1.5 - 157.5 J/cm2 (102). Some studies used light exposure within the mouth and others from the outside - and some combined the two. However, most studies use a dose between 1.5 and around 30 J/cm2 (102)! It's nevertheless hard to give a single protocol here due to the very different nature of what caused the injury, such as a tooth extraction or the plain post-surgical application of light therapy. Sensibility, pain, and recovery are nevertheless boosted big time with red light therapy.
- Another 2021 review also investigates the effects on the alveolar nerve (99). The studies pertained to alveolar nerve injury after a surgical procedure. Seven studies are included. Wavelengths used are 808 - 830 nm mainly, and the total dose is 3 - 244 J/cm2. Most studies showed recovery of the nerve and sensation. Treatment within six months of the injury led to the best results. However, far more data and more high-quality studies are needed for a proper assessment. With more data, more definitive conclusions can be drawn!
- A third review from 2020 investigates the use of light therapy after a jaw surgery - a correction of the lower jaw bone that supports the lower teeth (100). Eight studies were included. Light therapy wasn't effective within 48 hours after surgery but was very effective within 30 days. The jaw surgery in question here is the "bilateral sagittal split ramus osteotomy" - a complicated combination of words!
- Lastly, there's a 2021 review on the trigeminal nerve that's located higher up towards the jaw (101). Here are the very well-written findings and conclusion of the researchers:
"The reliability of [red light therapy applications] strongly bases on biological and physical-chemical evidence. Its principal player is the mitochondrion, whether its cytochromes are directly involved as a photoacceptor or indirectly through a vibrational and energetic variation of bound water: water as the photoacceptor. The 808-nm and 100 J/cm2 (0.07 W; 2.5 W/cm2; pulsed 50 Hz; 27 J per point; 80 s) on rats and 800-nm and 0.2 W/cm2 (0.2 W; 12 J/cm2; 12 J per point; 60 s, CW) on humans resulted as trustworthy therapies, which could be supported by extensive studies." (101)
Benefit 13: Counters Oral Mucositis Symptoms, Such As Pain And Inability To Eat
Oral mucositis is a side effect of cancer treatment. These treatments include radiotherapy and chemotherapy. As a result, you'll develop ulcers, swelling, pain, and difficulty swallowing.
Red light wavelengths in the 600s range with a lower total dose of up to 6 J/cm2 work best here. Red light lowers inflammation and oxidative stress. And, the incidence of oral mucositis can be lowered by more than 50% within a few weeks.
Oral mucositis is one of the areas in which the evidence for red light therapy for oral health is best by far. Oral mucositis occurs as a side effect of cancer treatment. With oral mucositis, you get ulcerations in the mouth (103; 104; 105; 106).
The resulting problem isn't just pain but the inability to eat or swallow. Redness and edema are other symptoms. As a result, quality of life can go down. And, often there's an increase in mortality.
A whopping 40% of patients undergoing chemotherapy develop oral mucositis (103). The number is also high with radiotherapy or the combination of radiotherapy and chemotherapy (105). With neck and head cancer patients, that number is as high as 90%. The reason for the development of mucositis is that the cell turnover is impeded as a result of cancer treatment.
Next up, let's check out what red light therapy for oral mucositis can do. I've found 5 reviews from 2024 alone (106; 107; 108; 109).
- The good news is that red light works super-well (106). A 2024 review included four of the highest-quality studies. The wavelengths used were 660 nm so that one is easy. There were strong effects on the salivary cytokines - messenger compounds closely tied to inflammation and oxidative stress. The severity of oral mucositis can be reduced. A super-low dose of 4 - 6.2 J/cm2 was used in these studies (110).
- Another 2024 review finds no effect of red light therapy in children - which is really sad (107). Honey did work, however, to shorten the hospital stay.
- One more 2024 review argues that there's still a search for the ultimate protocol for treating oral mucositis (108). Early treatment may help before the oral mucositis has developed into a more advanced stage. Early treatment may also be great for limiting all pain.
- Then, one more 2024 review (109). Here, the incidence was 51% lower in the light therapy group than in the control group after the second week of treatment. The results persisted up until 7 weeks. This review included 14 earlier studies. The risk of severe mucositis was also halved with light therapy treatment.
- Many other reviews have been published in earlier years as well - check out Heiskanen's Excel sheet if you want more info there!
Overall, red light therapy for oral mucositis is extremely promising!
Benefit 14: Aids Oral Surgery Outcomes
Oral surgery manages your gums, jaw, and the teeth itself (such as with implants). Two very common surgeries are connective tissue grafts and free gingival grafts. These two surgeries require a low dose in the 600s wavelength range of up to 6 J/cm2 for the best result. For a jaw surgery (orthognathic surgery) that corrects the jaw, doses of up to 100 J/cm2 are used in studies, but in part for painkilling.
Oral surgery refers to procedures within the mouth, gums, and jaw, often performed by a specialist like a periodontist or oral surgeon (111; 112; 113; 114; 115). Oral surgery conditions include tooth loss, gum recession, jaw alignment, and oral cancers. Two common types of oral surgery are connective tissue grafts and free gingival grafts. These surgeries treat gum recession, protect roots, and improve your smile (if you miss gum tissue, for instance!)
A connective tissue graft means you take tissue from under a flap of skin in the roof of the mouth (palate) and place it over an area with a gum recession. The connective tissue is transplanted under the existing gum tissue. Connective tissue grafts are popular due to their high success rate and natural appearance.
Next up, in a free gingival graft, tissue is taken directly from the top layer of the palate and applied to the area that needs more gum tissue. Free gingival grafts are often used for patients with thin gums, as they can strengthen the gum line but may have a slightly different aesthetic outcome compared to connective tissue grafts. Other oral surgeries include extractions, dental implants or crowns, and bone grafting.
So far, so good, the possibilities are endless - and expanding! Next up, let's explore what red light therapy can do for you here:
Red light therapy for oral surgery - here are the reviews:
- A 2018 review included four earlier studies (116). Here, adding red light therapy adds to the stability and predictability of a connective tissue graft. The problem, however, is that studies differ big time in their setup.
- Another 2018 review finds similar conclusions (117). Less gum recession (a lower probing depth) and a better attachment level on the teeth are found. More research is needed here, however, due to somewhat contradictory findings.
- Then, for the free gingival graft, there's a 2019 review (118). Here, two light therapy studies show significant improvements over placebo.
- Most wavelengths used in both procedures are found in the 600s range. The total dose is usually very low, at 4 - 6 J/cm2, although there are a few exceptions with higher power.
- Then there's also the "gingivectomy," where excess gum tissue is removed (119). Healing improved here after a few days compared to the control group, and pain was reduced. The total dose here is generally low again, at 2 - 4 J/cm2.
- Lastly, there are a few reviews on jaw surgery, also called orthognathic surgery (120; 121; 122; 123). The goal here is to change the jaw structure, such as a receding or protruding chin, for instance. Pain here is reduced with red light therapy, as is edema (120). Wavelengths used were between 660 and 940, with total doses of 5 - 100 J/cm2 (120). Light therapy is best applied within 48 hours of surgery (121). Maximum mouth opening is also improved up to a period of two months, implying better recovery (122). These studies do differ though, making the application of statistics harder (123).
Benefit 15: Boosts Orthodontics Outcomes
Orthodontics aims to correct the structure of teeth, jaw, and surrounding tissues. The field is evolving rapidly. Treatment includes braces, retainers, and aligners, among others, to correct problems such as malocclusions, teeth crowding, or overbites.
Different red light therapy studies for different goals, such as with orthodontic mini-implants or maxillary expansion, use different doses that I've included below. Most studies are positive, fortunately, such as for improved bone density and less pain.
Orthodontics is a huge rabbit hole and a whole separate field (124; 125; 126; 127; 128). The field is developing extremely rapidly, though, with AI, 3 printing, and other emerging tools (124).
Orthodontics aims to correct the alignment of your teeth and jaw. The goal is to correct dysfunction, such as malocclusions, and increase aesthetic appeal. Braces, aligners, and retainers are some of the tools used in orthodontics to adjust the structures. These correct overbites, or spaces, or an overcrowding of teeth (125). Those problems aren't just aesthetic, however, but can affect your breathing function, ability to speak, chew, and so forth! So, by correcting those problems, your overall health should also improve.
Orthodontics also influences your face in general. For instance, you can change the facial symmetry. And, often, orthodontists work together with other professionals, such as oral surgeons, for the best results (126).
Because this orthodontics field is large, I've limited myself to the most important topics. Here's what I found:
- First up, there are a few recent reviews on orthodontics mini implants (127; 128; 129). These are temporary implants made for the movement of teeth, in case a regular brace won't work. Here the stability of the implants is improved (127). Study setup varied widely, however, such as the wavelengths used or power density. A second review only finds a small improvement (128). A third review doesn't recommend light therapy either, at this moment, due to insufficient evidence (129).
- For orthodontics pain there are also a few really recent reviews (130; 131; 132). Both acupuncture and light therapy are great interventions for lowering pain after an orthodontic treatment (130). A second study shows how much the numbers decrease on a VAS scale, with 13 points after 6 hours and 23 points after 24 hours. That difference is huge. The VAS scale measures pain from 0 - 100, whereby "0" is "no pain" and "100" equals the worst pain imaginable. Another review has similar results (132).
- Next up, two reviews on maxillary expansion, with contradictory results (133; 134; 135). Two reviews find positive effects while one other doesn't. Maxillary expansion broadens your upper jaw and teeth. Most studies do seem to have benefits for bone formation, however, and potentially pain.
- In kids there may be benefit for root resorption - the breakdown of primary teeth so that the adult teeth can grow there (136; 137). These studies show positive effects. Studies use mostly near-infrared wavelengths with total doses of a max of 25 J/cm2 (138).
- For orthodontic tooth movement - the speed at which the position of your teeth changes with braces for instance - the results are also positive (139; 140; 141; 142). These reviews are all from 2023 and 2024. The 730 - 830 nm range seems to work well (139). Several benefits exist here, such as quicker bone remodelling, the stimulation of cellular activity, and shorter treatment times for orthodontics (140). Researchers recommend applying 4 - 6 J/cm2 to the root of the tooth (141). Light can be applied to teeth that need to increase their movement specifically (141). On review is extremely precisely with their recommendations, however:
"810 nm, 2.2 J per surface, 0.1 W in continuous mode/0.1 W average power in a super-pulsed, sweeping movement, 1mm from the mucosa, 22 seconds along the vestibular surface and 22 seconds along the lingual surface, the recommended speed of movement is 2 mm/sec, 1 application during each orthodontic control, to achieve dental movement acceleration and repeat the dose at 24 h to ensure pain elimination." (142).
That's it for orthodontics! Hopefully, we'll get even more research shortly!
Benefit 16: Counters Osteonecrosis (MRONJ)
Medication-Related Osteonecrosis of the Jaw (MRONJ) is a condition where jawbone tissue dies. This condition is often triggered by antiresorptive (for osteoporosis) and antiangiogenic (for cancer) prescription medications. If you've got cancer or osteoporosis, you're also more likely to be susceptible.
Next to regular medical treatment, red light therapy likely works for this condition. Good results have been found with Platelet-Rich Plasma and light therapy. More high-quality research is necessary on this topic for definitive statements, however!
Medication-Related Osteonecrosis of the Jaw (MRONJ) sounds complicated. The condition that involves the dying of jaw tissue occurs because of medication (143; 144; 145; 146). Antiresportive (osteoporosis) or antiangiogenic (cancer) medication is the main culprit.
However, the health condition isn't fully understood (143). Some patients with susceptibility due to osteoporosis or cancer have an increased risk (143). Children and young people are fortunately somewhat protected from MRONJ (144). The main issue is that the jaw's bone density goes down, leading to structural problems.
Symptoms of MRONJ include swelling, pain, infections, and openly exposed bone in the mouth. Treatment is difficult as there's no gold standard - rinses and surgical cleanings are the norm. Preventive dental care can also be used to lower the risk before starting the medications mentioned above.
Fortunately, red light therapy for MRONJ has a great risk-benefit profile (145; 146; 147):
- First, a review compares Platelet-Rich Plasma (PLP) and similar compounds with red light therapy - the conclusion is that the former is really useful (145). Laser technology is also helpful, as is "Photodynamic Therapy" (PDT), where light interacts with a compound. I support both strategies big time, as I've seen life-changing results with both. The full review text contains all the details of the treatment (148).
- A second review examines osteonecrosis in people with neck and head cancer (146). Here both light therapy and PRP are deemed to have insufficient evidence.
- A third review shows vast improvements in pain, with a 4+ point decrease on a scale of 0-10 (147). A score of "0" means no pain and a score of "10" the worst pain imaginable.
- Overall, more high-quality research is needed here but current studies do look promising! I see few Randomized Controlled Trials, for instance, which have a placebo and intervention group
Benefit 17: Improves Periodontium Health
Here I want to refer to my blog post on the topic - as it's far more in-depth than I can consider here: The Remarkable Role Of Light Therapy In Periodontal Care.
Periodontal health (your gums) takes center stage in oral health. Yet, many people have suboptimal periodontal health, with 90% of people having some inflammation of the gums. Also, half the US population has chronic periodontitis - a condition that is not benign because it often leads to further deterioration of oral health. Also, chronic periodontitis increases your risk of other conditions, such as heart and blood vessel disease and Alzheimer's
But here's the good news:
Red light therapy has a decent profile for treating the periodontal areas. I recommend using the LightpathLED Diesel Torch (code ALEX saves), which has an oral treatment tip. You'll have to treat each gum area for 50 seconds with the tip pressed against the gums for a 5 J/cm2 dose. That dose is very conservative and great for wound healing overall.
Your dentist, moreover, can also apply red light therapy in the clinic - especially when surgical or non-surgical periodontal interventions are used. Examples here are scaling and root planing, for removing plaque around the gums and under the gumline. Red light therapy has widespread beneficial proven effects in this case, such as for lowering inflammation, bleeding, and ensuring the pocket depth (the amount of gum loss) stays low. Red light therapy also lowers pain and increases healing speed.
Nevertheless, I still recommend combining red light therapy with lifestyle changes,. Examples here are proper nutrition, and regular dental checkups at the dentist, and plain and simple dental hygiene.
Benefit 18: Improves Temporomandibular Joint Dysfunction
Temporomandibular Joint Dysfunction (TMD) affects the jaw joint at the side of your face, as well as muscles located there. Jaw pain is quite prevalent as up to 30% of people experience TMD. If the condition isn't too bad, conservative treatment such as physical therapy can really help or medication. With more severity and TMD that lasts longer than a year, red light therapy can really work.
Red light therapy has recently shown promise in TMD management. You'll get pain reductions and improve jaw mobility, in dozens of studies. The issue is optimal finding red light therapy protocols, including ideal wavelengths and dosages. Here I recommend spot treatment, with an emphasis on near-infrared light, and using a trial and error approach with the dosing.
Temporomandibular Joint Dysfunction (TMD) is an issue with your jaw joint between the lower jaw and the temporal bone. The upper jaw doesn't move, so it's not directly affected. Often, muscles around the jaw are affected with TMD issues as well.
You can see a visualization of the Temporomandibular Joint (TMJ) here:
Contrary to how it may look, however, the TMJ is highly complex (149; 150; 151; 152; 153; 154). The disorder of the TMJ joint, the TMD, is also complex (149). Muscular issues can play a role, as can degenerative processes, disks, and joint issues such as osteoarthritis, as do other reasons. Just a correct diagnosis may thus already be difficult.
Physical therapy can help and has a decent evidence base - although I've never specialized in this joint as a physical therapist myself (149)! Conservative treatment works well initially.
If problems persist, however, especially longer than a year, you'll need treatment (150). If problems continue, you can have issues with clicking of the TMJ joint, or clenching, or locking (150). Pain is often the result, as well as difficulty speaking or chewing.
Up to 30% of adults have some form of TMD (152). For me that number is almost surprisingly high and seems somewhat impossible. When TMD progresses, surgery may be necessary. Researchers write:
"The evidence surrounding oral and topical pharmacotherapeutics for chronic TMD is low, whilst the evidence supporting injected pharmacotherapeutics is low to moderate. In concordance with current guidelines, moderate quality evidence supports the use of arthrocentesis or arthroscopy for arthrogenous TMD insufficiently managed by conservative measures, and open joint surgery for severe arthrogenous disease." (153).
The pharmaceuticals are the conservative treatment here and the physical therapy I just talked about (154). There's no ideal form of pain therapy, and a trial-and-error approach seems to work best - until people find a treatment that works for them (154).
Well, this is where red light therapy for TMD comes in! Here are the outcomes from a few recent reviews (155; 156; 157). One of these reviews is even written by a great dentist and researchers who I saw at PBM 2024 in London (157):
- First up, a review from 2023 has a wonderful write-up of the effects (155). I'll paraphrase the wording of the study here: A whopping 40 studies were included, and all but one measured pain. Here, 27 studies had lower pain scores in the red light therapy group versus the placebo group. The ability to open the mouth also improved in almost half of studies, and this was especially true for passive and active mouth opening (with passive you help to open your mouth, with your hands for instance). Movements to the side - so-called "lateral movement" - also improved in the studies that tested for it. The same is true for movement of the lower jaw to the front, which you need for chewing and other movements. And lastly, in 2/5 studies the sounds made by the jaw also decreased. So those are lovely results overall!
- A second 2023 review included 28 earlier studies (156). Here red light therapy worked well for pain, combined with a nightguard or without. People with TMD use a nightguard to stop grinding their teeth.
- Thirdly, there's the 2021 review by Prof Reem Hanna on RCTs for TMD (157). For the pain measured with the VAS scale, the lateral movement of the jaw, and the movement of the lower jaw to the front, red light therapy outperformed the control in most studies. However, more research is needed to differentiate the exact protocols for treating TMD, such as wavelength and total dose. Wavelengths varied in studies but are mostly found in the near-infrared range (158). Some studies used pulsing while others didn't. Most studies applied the laser directly to the skin. The total dose was "0.1 and 100 J/cm2/point", so that's a huge 1,000-fold difference. I'm oversimplifying here, but treatment is probably great at 2 - 3 times per week - this also varies in studies. The spot area treated in many studies is very small, at 2.8 cm2 at the maximum.
A LightpathLED Diesel Torch is probably great here (code ALEX saves). Or, alternatively, a handheld red light therapy unit. I'll say more about these devices in a later section.
Benefit 19: Eases Tooth Extraction Pain, Swelling, And Healing
Tooth extractions are a last resort when no other options are available. Natural teeth are often preferable, but need to be extracted due to trauma or caries, for instance. Implants are a decent option after tooth extraction.
I've discussed four reviews on light therapy after dental extraction here. The reviews have very different dosing and wavelength parameters, but generally, red light therapy is helpful for lowering pain, speeding up wound healing, enhancing mucosal repair, and boosting alveolar bone healing (the bone under the extraction socket). Swelling also goes down with light therapy but the effect isn't too strong.
The benefit here is that you can very easily apply the red light therapy, you can get a dose in under 60 seconds for pain, and often in seconds for wound healing.
Tooth extraction is something everyone hates. Between 36 and 55% of extractions are due to caries when the tooth is irreversibly damaged (159). Trauma and periodontitis are two other reasons for extractions.
Of course, you can rely on implants after a tooth extraction but natural teeth are always considered best - if they're healthy (160). Whether a tooth needs to be extracted or not depends on a complex decision making process (160). Tooth extractions aren't without risk either as complications can arise (161). One of these problems is bone loss, if an implant isn't placed in the location of the extracted tooth (162).
So what's the science on red light therapy for tooth extraction? There's a huge amount of science on this topic, fortunately, and here's what the reviews state (163; 164; 165; 166)
- The first 2024 review includes 18 earlier studies and mentions that these have too much dissimilarity in study setup (163). So, things like wavelengths and dosing protocols differ too much. The study investigates the removal of the wisdom teeth (third molars). However, mucosal repair and alveolar pocket healing are positive, as well as the pain scores (167). Alveolar pocket healing is the open area that remains after the removal of the third molars. Sometimes, alveolar osteitis is also reported, a side effect of improper healing after extracting these teeth, and outcomes are generally positive. There's generally insufficient evidence for bone repair and alveolar osteitis because more studies are needed.
- Another 2024 review investigates pain after a third molar removal (164). A total of 82 papers were included in the analysis, and 33 for the statistical analysis. Light therapy worked here for reducing pain, as did other strategies such as kinesio tape. Ozone therapy also worked after 7 days.
- A third 2023 review shows good effects on postoperative pain and wound healing (165). Twenty-two studies were included. Here's a good quote about the complexity of the different treatment parameters:
"Postoperative pain and [red light therapy] were reported in 20 articles for 24 treatment groups, with treatment times ranging from 17 through 900 seconds and wavelengths from 550 through 1,064 nm. Clinical wound healing outcomes were reported in 6 articles for 7 groups with treatment times ranging from 30 through 120 seconds and wavelengths from 660 through 808 nm" (165).
- So, treatment times and wavelengths vary wildly. The total dose also varies between roughly 2 and 212 J/cm2 for pain (168). The beam area is never bigger than 3.2 cm/2. For wound healing the total dose is 6 J/cm2 at the maximum.
- Fourthly, there's a 2023 review (166). Here a total of 33 studies were included. Pain, edema, and trismus (jaw joint restriction) were all lower with light therapy applied, but the effect wasn't huge, according to this review. Nevertheless, please remember that you can apply a good dose of light therapy in under a minute with a laser, so the small effect is still worth it, in my opinion.
Well, that's a good outcome! Light therapy doesn't have to seem a huge effect size but it's very easy and quick to apply. Also, as always, we need more and better studies, but these outcomes are already very promising.
Benefit 20: Boosts Oral Wound Healing
So here I have to refer to the article I already wrote on this topic, Oral Wound Healing With Red Light Therapy: Innovative Advancement?
But nevertheless a quick summary:
Oral wounds are different than regular wounds as they heal without scarring. So the physiology is different at a fundamental level. Also, the location of oral wounds is unique in that it interacts with many bacteria and other organisms in your oral cavity. So there are risks involved with oral wounds, such as infections or the spread of bacteria throughout the body.
Oral wound healing, as many oral outcomes, doesn't just depend on red light therapy alone. Many factors such as diabetes, stress, mouth breathing and nutritional deficiencies influence your risk of having poorer oral wound healing.
Traditionally, oral wounds are treated with ointments, pharmaceuticals, or other interventions, but these aren't perfect. Red light therapy can aid this healing process by improving energy production and lowering inflammation. As a result, collagen synthesis is higher and wounds heal quicker.
Both human and animal studies have investigated red light therapy's effect on outcomes such as incisions, gum lesions, and ulcers. The 660 - 670 nm wavelengths seem to be most effective here, although blue and green light have an effect as well. The total dose is best at 1 - 8 J/cm2.
I once again recommend the LightpathLED Diesel Torch in my blog, as well as the Noovalab Novoral Care Pro. Again, don't just rely on red light therapy as a panacea but see it as an addon tool instead!
And for a deep dive, read my oral wound healing article.
What Dentists Think About Red Light Therapy
Here I have to refer to my friend who is a dentist and oral surgeon, and regularly applied light therapy in her practice. I've written down some case studies of her, and her application fo light therapy. I'll update that document over time, with new topics added. Right now I only consider dentin hypersensitivity, bruxism, and the structure of the jaw there.
Light Therapy Devices For Oral Health
This section I'll also keep simple for now but update over time. I may even do some testing of some dental products. The main products I want to recommend are the following - if you're buying a device for dental health only.
First up, there's the handheld red light therapy units:
These handheld units can be used on the skin, such as the jaw area, and are quite versatile. You can use these handheld units for many other purposes, such as treating a tendon in your body or for muscle recovery. The handheld units are poor for treating areas in your mouth, however.
Which is why currently the LightpathLED Diesel Torch is currently the top device out there that I recommend (discount code ALEX saves if you buy):
And, thirdly, if you want a device that's easy to use while freeing up your hands, consider the Novoral Care Pro below:
All of these devices have been reviewed by Alex Fergus. I recommend you watch the reviews and buy based on these!
Lastly, I want to give an honerable mention to Thor Lasers (mention Alex Fergus for a potential discount!). Thor Lasers is the absolute best option if you want a red light therapy (formally known as "photobiomodulation") device as a clinician. For dentists, there are several tools in here, such as an oral probe, a lollipop, and several that can be used on the lips, cheeks, jaw, face, or neck area.
Dosing Red Light Therapy For Oral Health
How to dose red light therapy for oral health? Here are the input numbers you need:
- The handheld red light therapy units I talked about will generally have a dose of 40 - 50 mW/cm2 at 6 inches.
- The LightpathLED Diesel Torch - discount code ALEX saves - has an 100 mW/cm2 dose at the oral tip, when it's directly pressed against the skin.
- The Noovalab Novoral Care Pro - use discount code ALEX15 to save - is dosed automatically with its inbuilt timer.
- Thor Lasers - the product comes with excellent instructions and even a course that I've been to. You can mention Alex Fergus for a potential discount here!
Please check the following blogs on how to aply that light and dose properly:
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
I really wish I could make this all much simpler - but until we've got specialized devices for many of these goals (benefits) I've listed above, you'll have to calculate the dose manually to get the scientifically-backed dose! This will get better in time, but for now, it's time consuming...
Finally, let's conclude:
Conclusion: Join The Red Light Therapy For Dentistry Revolution
Whether it's red light therapy for teeth or red light therapy for gums, or adjacent structures, the science on this topic is extremely promising. I'll be following the scientific literature on this topic in the coming years and may publish a new version of this blog in, say, 5 years.
The good news is that almost regarless of topic, whether it's using light therapy for gum disease, or for dentin hypersensitivity, or tooth extractions, there's often some level of evidence present. And that's great for a field that's exponentially exploding right now, with the number of yearly publications.
I've tried to simplify the topic as much as possible here. And, unfortunately, the literature is still complex and no easy answers are possible! I will also say, in the end here, as I've stated many times, is that there are no replacements for focusing on your general health. Examples are - from my dentin hypersensitivity article:
- Flossing once per day and brushing, ideally with 10% hydroxyapatite natural toothpaste.
- Visit your dentist twice per year for a checkup and cleaning.
- Eating a well-balanced diet (get something that works for you, whether a Ray Peat diet or Paleo or whatever!).
- Get good quality sleep.
- Fix mouth breathing, which is horrible for dental health.
- And so forth. There are no magic bullets here, and red light therapy isn't one either. Red light therapy will nicely move the needle, however, especially in the coming years once you and I find out about new, more successful protocols!
Limitations
Finally, though, I do want to mention a few caveats or limitations:
- Side effects are rare or non-existent but in some cases,, you'll still have to consult your physician, such as in the cases of cancer, autoimmune disease, or multiple chronic diseases. I can't rule out all side effects. And, in some cases, such as cancer, red light therapy may be outright contraindicated, especially without your doctor's approval.
- More long-term studies are needed - but these are prohibitively, expensive! Some of the gurus in our space, such as Prof Dr Michael Hamblin, believe that you'd see far more significant benefits when participants aren't just followed for a few weeks but for months ore even years. But, studies can already cost into the millions as of now, so funding is needed here! You'd probably also find benefits with long-term studies that not found in the studies listed above.
- Study quality could be higher sometimes - but that's to be expected. For instance, higher number of participants inside these studies would make them better. The issue, here, once again, is funding. Including more participants is more expensive. And, finding good funding for these studies is difficult because light is harder to patent - it's part of nature. So you can't exect return in the long run like you can on pharmaceutical drugs, even when succesful.
Frequently Asked Questions
Here I consider a few frequently asked questions about red light therapy for dentistry:
What Is Red Light Therapy, And How Does It Work in Dentistry?
Red light therapy is usually applied with a laser, for dentistry, by a dentist. However, in some cases such as oral wound healing, or gum recessions, or whitening of the teeth, it's possible that you yourself apply the light therapy and get the benefits.
Check my full article for the nuance on these many topics!
Is Red Light Therapy Safe For Dental Treatments?
Red light therapy is safe for dental treatments, as there are almost no known side effects in the literature. The only side effect to be careful with is oral cancer - consult your physician before using red light therapy in that case.
Generally, however, the most important factor to avoid any side effects is to stay within the dosing guidelines I've outlined in my article above, for each of the specific goals.
Does Red Light Therapy Work For All Types Of Dental Patients?
For almost all types of dental patients, red light therapy seems to work. Some topics are less explored, however, such as the effect on caries. Other topics, such as jaw joint pain or periodontal disease, have lots of science backing it.
But, seeing the scientific literature as a whole, for most goals, whether red light therapy for gum recession, or red light therapy for mouth ulcers, or red light therapy for canker sores, the effects are positive.
How Long Does A Typical Red Light Therapy Session Last In Dentistry?
With a high-powered laser, a session typically lasts around a minute at your dentist. If you're treating your teeth or gums or other tissues at home, it may last from a few minutes up to 10-20 minutes. However, devices exist that you can put in your mouth for oral treatment!
Items Mentioned In This Article
- Noovalab Novoral Care Pro - use discount code ALEX15 to save
- LightpathLED Diesel Torch - discount code ALEX saves
This is a post by Bart Wolbers of Light Therapy Insiders. Bart finished degrees in Physical Therapy (B), Philosophy (BA and MA), Philosophy of Science and Technology (MS - with distinction), and Clinical Health Science (MS), has had training in functional medicine, and is currently chief science writer.
Found This Interesting? Then You Might Like:
- Start Here - Light Therapy 101 & Buyers Guide
- Discount Codes, Deals & Recommendations - Red Light Therapy
- Oral Wound Healing With Red Light Therapy: Innovative Advancement?
- Dentin Hypersensitivity: Why Red Light Therapy Is A Game-Changer
- How Red Light Therapy In Dental Anesthesia Practices Shows Great Promise
- The Remarkable Role Of Light Therapy In Periodontal Care
- Dental Red Light Therapy Before And After Case Studies From Clinical Practice









