We're getting questions about red light therapy and hyperpigmentation super frequently in our massive Facebook group on red light therapy:
"Hey Bart, I used red light therapy panels for a week and now my hyperpigmentation has gotten worse. What should I do?"
Or, you'd get comments like "I used devices, X and Y for the last three months and my melasma has massively improved"
And for many people, there are simply no changes at all - me included. No matter what I do with red light therapy specifically or light therapy in general, I don't get any "brown spots" on my skin.
So in this article, I decided to do a massive deep dive into red light therapy for hyperpigmentation. Melasma is one form of hyperpigmentation. I'll start with an introduction, and then talk about sunlight and hyperpigmentation, then cover all available studies on the topic, and finally consider other factors that are very often overlooked on the topic. And if you're short on time, just read the summary below:
Red Light Therapy For Melasma & Hyperpigmentation Summary
Several types of hyperpigmentation in the skin exist, and melasma is one of them. These types of hyperpigmentation are characterized by the buildup of melanin in the skin, which gives it its dark appearance. Melanin protects your skin against ultraviolet light (which can give you sunburns), but it has far more functions as it soon becomes clear!
Different types of hyperpigmentation have different characteristics and causes. The Fitzpatrick classification system for skin types is invaluable here, with classes I (very light skin) to VI (very dark skin). Darker skin types of Fitzpatrick type III and above have higher melasma risk.
Generally, when I look at the scientific literature, blue and ultraviolet light increase melanin levels in the skin. Amber, red, and near-infrared counter that pigmentation. My surprising finding here was that red and near-infrared counter melasma, even when used at higher intensities and at higher doses! Red and near-infrared light inhibit melanin production, inflammation, and abnormal blood vessel growth (melasma exhibits this!).
What is underestimated in almost any hyperpigmentation and melasma article on the internet are many other lifestyle and nutrition factors that protect against potential blue and ultraviolet light damage on the one hand and promote skin health on the other hand. Vitamins A, C, E, DHA, collagen protein, and other nutrients can protect against skin damage and make it healthier but few people talk about that topic. And yet, with modern diets, many people are deficient in these - only health "freaks" nowadays take sufficient DHA and collagen, for instance!
The nutrient argument I've "borrowed" from neurosurgeon Dr. Jack Kruse - whose work I've been reading for over a decade now. Dr. Kruse also discusses the link between circadian rhythm disruptions, mitochondrial health, and melasma or hyperpigmentation. Dr. Kruse also talks about how artificial blue light indoors for hours a day creates a totally abnormal stimulus for the human skin that our ancestors didn't have for millions of years!
In conclusion, I favor a more holistic approach to managing hyperpigmentation and melasma. I don't think there's a single factor creating problems here, and I'm even happy finding no convincing evidence that red or near-infrared causes melasma or hyperpigmentation - even at higher power outputs - because the studies show that these can be used to impede the condition!
Other Important Comments
If you need an introduction to what these terms mean, check the following resources:
- What Is Red Light Therapy?
- Red Light Therapy Explained: Basic Terms Guide
- Start Here - Light Therapy 101 & Buyers Guide
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
- How Often Should You Use Red Light Therapy Explained
These resources should give you a basic understanding of how red light therapy works, and the discussions around it!
What Is Melasma And What Is Hyperpigmentation? An Introduction
Melasma is a type of hyperpigmentation characterized by locally increased melanin. The result of that melanin is a dark patch on the skin. Melanin protects your body against ultraviolet light, which most people get exposed to from sunlight.
Different types of hyperpigmentation exist - such as drug-induced or post-inflammatory hyperpigmentation. Hyperpigmentation can occur from several causes, such as trauma, (sun)light exposure, or appearsskin conditions. Melasma, however, occurs more after hormonal imbalances, pregnancy, and ultraviolet light exposure. Melasma is more common if you have dark skin, while the other types of hyperpigmentation are more frequently found in people with lighter skin.
The darkness of your skin (as well as other factors) determines your Fitzpatrick type. The lower that Fitzpatrick number (running from I to VI), the lighter your skin is. A darker skin entails having more melanin and hyperpigmentation is generally less visible on that skin.
Most hyperpigmentation affects people's quality of life. Treatment can be complex and is not always predictable. Treatment often consists of prescription medicine, topical applications, light therapy, microneedling, and other therapies. Pharmaceutical and topical treatment aren't always without side effects.
Dark skin patches characterize both melasma and hyperpigmentation. However, the causes for both are different, as well as how they look and how they are treated.
Why Hyperpigmentation Matters
As you can imagine, hyperpigmentation and melasma - so you are developing brown spots - aren't optimal from an aesthetic perspective. These different brown spots directly affect the quality of life (1; 2; 3; 4).
The reason here is that with your aesthetic appearance is affected, your quality of life goes down. That effect seems present across different cultures! However, people with Fitzpatrick type III and IV are most commonly affected. These are people with generally lighter skin types.
Let's explore that topic:
Melanin, Skin Types, And The Fitzpatrick Classification System
Now, hyperpigmentation and related disorders is closely related to the Fitzpatrick Classification System. The Fitzpatrick Classification System or Scale was developed decades ago to differentiate between skin types (5; 6; 7; 8; 9in ). Here, type I has the lightest, and type VI has the darkest skin type. I'll come back to the topic of hyperpigmentation below and first introduce this classification system:
Lighter skin generally has less melanin, which gives you that classic tan. That melanin is also involved in the creation of hyperpigmentation, however, because it's a local buildup of melanin.
So when the sun is higher up in the sky, ultraviolet light is emitted. Your skin protects itself by ultraviolet light by producing melanin. That is a normal process that's extremely healthy and good - I'll come back to that topic in great detail later in this article though!
Fitzpatrick types V and VI naturally have higher melanin levels and don't need lots of exposure to ultraviolet light to have higher melanin levels already. And conversely, Fitzpatrick type I has very limited ability to create melanin and will very easily burn.
These are almost certainly adaptations to different environments (10; 11; 12; 13). People with a lighter skin type more easily create vitamin D in the skin–but they also sunburn much quicker! That vitamin D mechanism may be one of the reasons why people moving further away from the equator eventually got lighter skin. From a genetic perspective, however, this process is complex (13).
Type I: Very white skin that burns very quickly and never tans. I had a friend with brown hair and very pale skin for many years, who could only tan by using very strong British tanning beds consistently over time. At type I, you're also at higher risk for sun damage.
Type II: Mostly white skin but not pale white, that still easily burns. Fortunately, at this type, you can tan but that is more difficult. Here, you are still at higher risk of sun damage.
Type III: More cream or bronze skin (when tanned), that is better able to create melanin. I'm this type, probabaly! Still, there is the risk of sun damage but you can gradually tan over time to prevent that damage.
Type IV: Here's where we are at a the lighter brown skin type - many people in Latin America have this type, such as where I'm living currently in Paraguay. These people can tan very easily but can also still burn, and nevertheless, they often make me jealous because they look so much different after a sunny day! Here, the risk of sun damage also decreases.
Type V: These are the people with darker brown skin, who rarely burn. These skin types are primarily found in subtropical and tropical areas, building melanin super quickly. Burning is extremely rare.
Type VI: Finally, you've got people with dark brown or black skin who never had sunburn and tan exceptionally well. Here the risk of sun damage is also super low, so you don't need to be as careful with staying out in the sun too long.
Lastly, generally, people with lower Fitzpatrick types have lighter eyes (such as blue and green), and people with higher types tend to have darker eyes. I say "tend" here because I've also seen darker-skinned Brazilians with blue eyes and Germans with brown eyes. So it's only a general pattern.
However, the Fitzpatrick Scale can be made even more complex with additional information such as whether you have sensitive skin and scarring risk (6). Other differences play a role as well (7).
Nevertheless, more sunlight exposure specifically (or ultraviolet light in general) is not always benign (8). Darker skin types seem to have higher skin cancer risk - at Fitzpatrick types IV-VI - because of a false sense of security.
However, you're fortunate with the darker skin types because hyperpigmentation or melasma is much less visible. The reason for that lower visibility is the contrast - a darker brown spot on light brown or black skin is visually more challenging.
Different Types Of Hyperpigmentation
So, back to the topic of hyperpigmentation (14; 15; 16; 17; 18; 19; 20). Here, researchers write:
"Disorders of hyperpigmentation are common and, depending on the extent and location of involvement, can affect the quality of life and pose a significant psychologic burden for patients. Given the similarities in presentation of the various causes of hyperpigmentation, it is often difficult to [retrace the link of cause and effect for] these conditions, which is important to guide management. Furthermore, certain disorders [...] have similar clinical and/or [cell-science based] presentations, and their classification as distinct entities has been debated upon, leading to additional confusion" (14)
There are also a few different types of hyperpigmentation:
- Post-inflammatory hyperpigmentation - which appears after an injury. I've got a few scars on my legs, for instance, that have hyperpigmentation now! Skin conditions such as eczema and acne can also cause post-inflammatory hyperpigmentation.
- Sun spots or age spots - well, you probably know people who have spent tons of time in the sun and have developed these! I'll consider this topic in more detail later, but in my opinion these issues aren't just caused because of excess sunlight exposure, but often because of poor repair mechanisms such as through an unhealthy diet. I won't focus too much on these in this blog post.
- Drug-induced hyperpigmentation - created as a side effect of different pharmaceuticals. Simple, as the name already implies!
- Melasma - caused by pregnancy, hormonal changes, or drugs. So it's important here to note that not all hyperpigmentation is melasma - they're not the same thing! The melasma is also commonly found on the face, not across the entire body such as hyperpigmentation in general or sun spots or scar tissue specifically do. I'll mostly focus on melasma in my blog because we get so many questions about this in our Facebook group.
No matter what your Fitzpatrick skin type is, you can be affected by hyperpigmentation. Treatment, however, differs according to the cause.
Different types of hyperpigmentation affect either the more superficial parts of the skin (the "epidermis") or deeper layers of parts (the "dermis") ( (14). Treatments are also not without risk and can exacerbate the problem (15).
Different types of melanin also exist - eumelanin and pheomelanin (16). The first is the black-brown melanin give your skin a dark color and the second is red-yellow responsible for red-yellow leaning skin colors and the red hair color.
The first is protective against ultraviolet light while the latter is not. And depending on your lifestyle, nutrition, pharmaceutical intake, and more, the body can shift more towards one or the other melanin production (16).
Then there's the issue of treatment. Hydroquinone has been used for many years to counter hyperpigmentation such as melasma and post-inflammatory hyperpigmentation (17). Hydroquinone works really well to lighten spots in the skin locally.
However, hydroquinone is also linked to side effects now (17)! At best, you get some skin irritation, such as swelling or a rash. At worst, the compound can lead to neuropathy, sun sensitivity, and systemic effects because everything you place on the skin affects the body as a whole and potentially increases cancer risk.
Nevertheless, there are some common sense interventions for lowering the risk of hyperpigmentation. Examples here are to avoid pollution and not smoke (18). Alcohol and drug abuse can also cause tons of different hyperpigmentation conditions, as well as skin conditions in general (21; 22; 23). Aging also puts you at higher risk (18).
Melasma
Melasma may be relatively unique because of the strong hormonal influence and that of pregnancy (19). Surprisingly, the Fitzpatrick IV-VI types are most likely affected by melasma - so the people with darker skin!
Different types of melasma exist, such as the upper skin layer (epidermis), the lower skin layer (dermis), or a mix between them. In my opinion, ton because of the mechanisms involved. Researchers write here that the issue is caused by:
"(1) skin barrier dysfunction and abnormal synthesis, transport, and intracellular distribution of melanin in the epidermis; (2) basement membrane damage; (3) solar elastosis, vascular changes, senescent fibroblasts, mast cell infiltration, and sebocyte participation in the dermis; and (4) systemic factors such as sex hormones and oxidative stress" (24).
While that quote sounds complicated, your nutrition and lifestyle influence many factors. For instance, the stuff you put on your skin can affect skin barrier dysfunction - the general rule here is not to put anything on your skin that you wouldn't eat. Oxidative stress is strongly affected by your overall lifestyle, such as nutrition, sleep quality, whether you exercise and move, etc. The same applies to your hormones and vascular (blood vessel) changes.
Seeing this evidence, it's extremely unlikely that melasma is caused only by light exposure or the interaction between hormones (such as in pregnancy) and light exposure. Substantial changes in the skin physiology and related tissues are found in melasma (25).
Here's the current science on melasma treatment:
"Triple combination cream (hydroquinone, tretinoin, and corticosteroid) remains the most effective treatment for melasma, as well as hydroquinone alone. Chemical peels and laser- and light-based devices have mixed results. Oral tranexamic acid is a promising new treatment for moderate and severe recurrent melasma." (26).
The best fix here, however, is combining prevention with treatment of existing melasma (27; 28; 31). Many of these studies mention avoiding ultraviolet light, but that's no solution, in my opinion, because you need ultraviolet light exposure for optimal health, in my opinion (27; 28). That solution is like telling people they shouldn't move anymore because they have knee osteoarthritis. Not moving will have a huge impact on your general health, just like avoiding the sun does.
Melasma does affect a huge number of people - between 8.8 and 40% of the population, depending on the geographical area (29). And just like hyperpigmentation in general, melasma affects quality of life. Permanent solutions are rare, so the condition re-occurs frequently (29). Hence, solutions are desperately needed here!
Fortunately, there are some new therapies that use far more natural means to counter melasma, such as Platelet-Rich Plasma (PRP) (30). PRP is derived from your own blood and I've seen "miracles" happen with that therapy. I talk about many other strategies later in this article...
Treatment Of Different Types Of Hyperpigmentation
And, simply because not all hyperpigmentation is created equal, the solutions are also not the same. I've already explored melasma above - so here's a brief review of hyperpigmentation treatment in general:
- Post-inflammatory hyperpigmentation - is caused by melanin buildup after earlier skin conditions, trauma, and as a side effect of dermatological therapy (32; 33; 34; 35; 36). Lasers can help here - which I'll come back to later in this article, but don't always work well (33)! Topical treatments with pharmaceuticals, however, are more generally the first line of treatment (34). Post-inflammatory hyperpigmentation mostly affects people with Fitzpatrick types III and IV - so those with an average amount of melanin. There's far less consensus on how to avoiding post-inflammatory hyperpigmentation rather than treating it (34). Early treatment after an insult to the skin is likely extremely important (35). That early treatment consists of medicine, topic agents, and light therapy right now.
- Sunspots, also known as "Solar Lentigines" or "aging spots" - which you get from excessive sunlight exposure or improper repair mechansims, is well-treated by light therapy (lasers) (36; 37). Cryotherapy, so the application of cold, may also work (38). And topical agents are used again (39; 40). I wish I could find more studies on laser treatment here!
- Freckles, also known as "Ephelides" - which mostly affect the Fitzpatrick type I and II skin types. Freckles are well-treated with lasers (41; 42; 43). Topical agents, whether that's chemical peels or simple vitamins such as vitamin A can work here.
- Drug-incuded hyperpigmentation is also once again treated with pharmaceutical and topical agents (44; 45). Often, this condition is harder to diagnose because people may be on several pharmaceuticals.
And, with that, I've hopefully given you a good introduction into what hyperpigmentation is and its different forms! Let's take a deeper dive into the topic of sunlight below:
Sunlight And Skin Hyperpigmentation
Traditional science envisions both ultraviolet and visible (mostly blue) light as the culprit for hyperpigmentation. Sunlight is the main form of exposure here. Most scientists recommend avoiding the sun and wearing highly protective (SPF 25+) sunscreen when you do.
However, there's convincing evidence that many nutrients, such as vitamins A, C, and E, and vitamin A precursors (carotenes and others), as well as compounds from fish such as fats and antioxidants, and collagen-like proteins in the diet have a highly protective effect. So it's likely that hyperpigmentation risk also goes up if the body cannot repair itself due to a poor diet, which most of the world now follows.
Lastly, there's more complexity here. Near-infrared light can protect your skin against damage, for instance. Modern indoor lighting environments with a ton of blue light exposure offer a very imbalanced exposure to the skin and eyes. And, many people go outside without getting any morning sun, thereby setting themselves up for problems because their skin is not preconditioned by red and near-infared from the morning sun!
With many of these conditions I mentioned above, there's a strong link to sunlight exposure in much of the research (46; 47; 48; 49; 50; 51). That conclusion is paired with the advice to universally wear sunscreen if you're out in the sun.
I'll get back to these statements in a moment. And the problems aren't just attributed to ultraviolet light. Here's what researchers recently state:
"The negative effects of sun exposure have become better accepted among health care professionals and the lay public over recent decades. Most attention has been focused on the effects of [Ultra-Violet (UV)] light, particularly [Ultraviolet B (UVB)] wavelengths (290-320 nm). Accordingly, products to protect skin from sunlight-associated harm (sunscreens) have been developed to minimize UVB exposure. The effects of longer wavelengths, including UVA (320-400 nm) and visible light [(Visible Light (VL)], 400-700 nm), are increasingly appreciated. VL accounts for approximately half of the solar radiation that reaches the earth's surface and understanding of its effects on the skin is improving. Studies have shown that VL can induce hyperpigmentation in individuals with dark skin types (Fitzpatrick skin types IV-VI). In addition, VL can contribute to the exacerbation of pigmentary disorders, including melasma." (46).
So, it's different types of ultraviolet light as well as visible light that is are the culprits for hyperpigmentation, according to researchers! The conclusion is very interesting, to say the least, given our ancestral past.
If you believe in evolution (I do strongly), humans would have been exposed to powerful sunlight around the equator for hundreds of thousands of years. And even millions of years when you include all ancestors.
Fortunately, recently there has been a stronger focus on endogenous sunscreen compounds that protect your skin (47; 52). Studies mention compounds such as vitamin C, vitamin E, carotenoids (vitamin-A precursors), and polyphenols (found in plant foods). But, these are once again suggested as additives to sunscreen that you add to the skin.
And, yes, I would agree that more natural sunscreens are a big win. I'm a massive fan of zinc-oxide-based sunscreens if you do need to use them. For most people, it's better to cover up with long-sleeve clothes and a hat - which the locals wear in the tropics where I live. Or to go into the shade!
Infrared light can be used to precondition the skin, for instance, which protects against ultraviolet light (53). You can see the effects in Figure 5 of that study below:
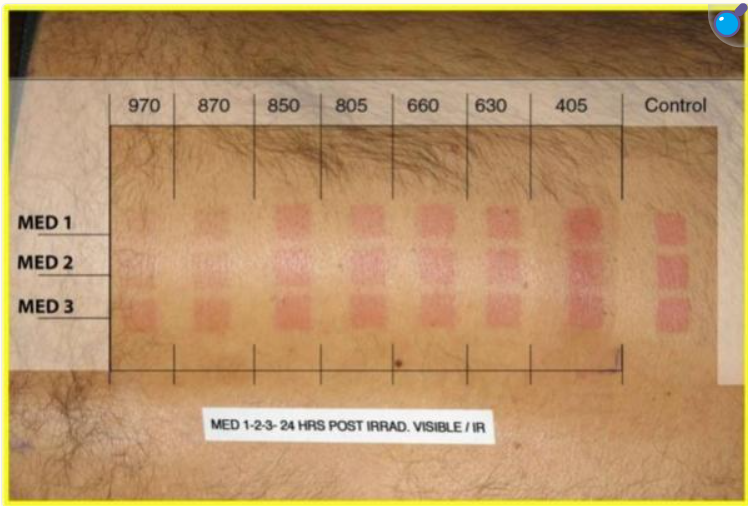
So, near infrared between 805 and 970 nm looks very protective against skin reddening. But this topic is seldom talked about by proponents who tell you to limit sunlight exposure.
And no, I'm not advocating that more is better with sunlight exposure. The optimal pattern is likely more like exercise, where no exercise is insufficient for you, and 8 hours per day is also bad for you. Just like sunlight exposure, exercise causes temporary stress and damage to the body (54; 55; 56). You get temporary inflammation, muscle damage, heightened stress hormones, DNA damage, oxidative stress, and more - but that doesn't mean that all exercise is bad for you! Exercise is only bad for you if you damage yourself permanently.
And, just as is the case with exercise, nutrition is of vital importance for not only skin health but also for dealing with the temporary damage created by ultraviolet light. Here are some examples:
- Collagen, gelatin, bone broth, and related food groups protect against ultraviolet damage (57; 58; 59; 60). Modern humans almost don't consume these proteins anymore, even though they are incredibly unique in their function. These proteins don't just make your skin look better–they also protect your skin.
- Docosahexaenoic acid (DHA) - a compound found in oily fatty fish - also protects against ultraviolet light damage (61; 62; 63; 64). You can find DHA in shellfish, shrimp, and fish like sardines, mackerel, herring, anchovies, wild salmon, and so forth!
- Carotenes (vitamin A precursors), and similar compounds such as lutein and zeaxanthin, and vitamin A, protect against ultraviolet light damage (65; 66; 67; 68; 69; 70; 71; 72). Just eat a wide variety of unprocessed animal and plant foods to get sufficient vitamin A and vitamin A precursors, as well as other compounds.
- Vitamin C and E are also super important for skin health in general– and protect against ultraviolet light damage (73; 74; 75; 76; 77; 78; 79; 80). This includes eye damage, another concern many people have with blue and ultraviolet light exposure!
- More compounds can be named here, such as green tea extract, astaxanthin (an antioxidant primarily found in seafood), and others. The main issue here is that you'll have an overall healthy diet of unprocessed foods because, likely, many of these protective compounds haven't been identified yet, and you'd be missing out on them if you focused on supplements.
And, yes, there's a lot more research needed on these compounds. But, likely,as one main reason why people do so poorly with photoaging of the skin and have high ultraviolet light damage is because diets across the world have become extremely poor.
Again, just as you can't expect excellent exercise recovery when you're not eating normal food, the same is likely true for protection against (temporary) ultraviolet and blue light damage. Yes, the word "normal" is a bit provocative because many people in developed nations don't eat food that can be considered "normal".
Nevertheless, so far, so good!
Then there's the issue of electronic devices and indoor lighting, which creates a highly unnatural human environment, with a considerable emphasis on blue light (51; 81; 82). It's likely not the dose that causes the poison here, but the unnatural exposure form - with the absence of the healing red and infrared parts of the light spectrum. I'll get back to that topic in great detail soon!
Overall, the fix here is to fix your diet and indoor lighting environment, and ensure you're getting some morning sun or red light therapy before going into the strong ultraviolet light environment midday. Also, it's very unlikely in my opinion that sunlight alone is responsible for hyperpigmentation and melasma!
Why use red light therapy? The latter is similar to exercising without warming up - your risk of injury goes up dramatically.
I'll come back to a related topic later in this article - first up, let's consider the few melanin studies that are out there below:
Light Therapy And Melanin Studies
Prof Dr Hamblin, whom I met in the past, has reviewed the science and shows that tyrosine (an amino acid) and hormonal pathways lead to melanin formation in the skin.
In mice and in vitro studies, ultraviolet and blue light stimulate melanin formation. Green, yellow, red, and near-infrared inhibit melanin formation in almost all studies.
We need far better human studies here, however! And more of them. But so far, red and near-infrared seem safe for hyperpigmentation and melanin and won't cause it, even with higher power outputs!
So, there are nine light therapy and melanin studies in total. I've included these as they may tell you more about how melanin interacts with light. I've included all nine studies, and I've not cherry-picked any of them - although some of them may be less applicable than others:
Reviews (Highest Level Of Evidence)
- Then there's a review on light therapy and melanin (83). That review is written by Prof Dr Michael Hamblin who I met at PBM 2024 in London (84). Here's my take on Prof Dr Hamblin's thesis here in great detail:
- Prof. Dr. Hamblin explains that melanin production relies on the amino acid tyrosine - which is also related to dopamine. Dopamine aids abstract thought and makes you motivated. The Tyrosine is also taken up by "keratocytes," or skin cells. However, the creation of melanin in the skin relies on several hormones. These are alpha-melanocyte stimulating hormone (alpha-MSH) and its related pro-opiomelanocortin (POMC). Ultraviolet light is the primary mechanism for this process (84).
- However, there can be disorders of pigmentation (84). Prof Dr Hamblin acknowledges that these disorders, such as hyperpigmentation, can be problematic aesthetically, but they rarely matter from a health standpoint.
- According to Hamblin, light therapy may help treat age spots as well as melasma. Light therapy can also be used for hypo-pigmentation in situations where there's too little melanin, such as Vitiligo. And, Prof. Dr. Hamblin states that light therapy is widely used in the cosmetic industry precisely because it works and is safe and non-invasive. Here, I want to quote Prof Dr Hamblin's own words:
"[Red light therapy] has been widely employed for skin rejuvenation and cosmetic dermatology, especially on the face, mediated by various wavelengths and power densities of light-emitting diode (LED) devices. In addition to the expected effects on collagen production in dermal fibroblasts leading to a reduction in fine lines and wrinkles, beneficial effects on hyperpigmented spots have also been observed.
[...]
,
[Red light therapy] using fairly similar parameters may, therefore, be able to produce opposite effects in the skin, either lightening it or darkening it depending on what is required for optimum cosmetic outcomes."
- I'll come back to the specific studies used by Hamblin later. So far, we're in hopeful territory, though! I'm assuming here that the parameters are blue/ultraviolet on the one hand, and the other colors on the other hand - given all the publications on this topic that I consider below!
- I can't find any human studies on this topic right now - but likely these were included in the "melasma" category that I'll consider later!
Mice Studies
Here are mice studies, which cannot always be extrapolated to the outcomes in human studies:
- There's a mice study where the mice wear a LED device that inhibits melanin creation (85). The problem here is that there's no info about wavelengths, or the nature of the device, or treatment parameters in general!
- Then a 660 nm mouse study (87). The alpha-melanocyte-stimulating hormone (alpha-MSH) I discussed, before from the review of Prof Dr Hamblin was inhibited. Here too, the 660 nm leads to depigmentation. The full picture is complicated though, as ultraviolet-B was also included:
"These findings suggest that the depigmenting effects of 660-nm LED result from downregulation of MITF and tyrosinase expression due to increased ERK activity. The 660-nm LED reduced UVB-induced melanogenesis in the skin of HRM-2 via downregulation of tyrosinase and MITF." (87)
- So, these processes are really complex. Nevertheless, even if the biological mechanisms aren't fully understood, 660 nm does inhibit melanin formation! Good news!
In Vitro Studies (Lowest Level Of Evidence - But May Be Useful!)
In vitro means "in the glass", literally, and these are foundational laboratory studies. You can imagine a petri dish study from science class in high school as an example.
Here's what was found concerning melanin in in vitro studies:
- First up, an in vitro study with 830 nm (81). Here, the 830 nm light counteracts the activity of proteins related to the creation of melanin. And the result is decreased pigmentation. A total dose of 5 - 20 J/cm2 was used.
- Then, another study showing that blue light induces skin pigmentation (82). The mechanisms here are quite complex, such as Opsins in the skin and TRPV1, which affect calcium signalingpretty. The bottom line here is that melanin production is finally stimulated.
- Yellow light at 585 nm can inhibit melanin synthesis in an in vitro study (86). Tyrosine activity was reduced.
- One more 585 study has similar findings (87). What's interesting is that a higher dose of 585 nm has a stronger effect on impeding melanin. Both 5 and 20 J/cm2 were tested in this study, but keep in mind that in vitro studies are very hard to extrapolate to human outcomes!
- Then, a study with 355 nm ultraviolet light, 457 nm blue light, and 635 nm red light (88). This study contradicts earlier studies and shows that even red light increases melanin formation! This is the only anomaly I've found!
- Lastly, there's one more study with 830 and 850 nm (89). Both wavelengths decreased melanin formation!
Overall, it seems that blue and ultraviolet light tend to promote melanin synthesis more. And the green, yellow, red, and near-infrared light tends to inhibit melanin genesis!
We need far better studies here, though. There are no high-quality human studies in this case, for instance!
Light Therapy And Melasma Studies
I went through all available clinical studies on light therapy for melasma, and generally, the outcome here is very positive! Different types of amber, red, and near-infrared can lower the melanin level in the skin, redness, and blood vessel growth near the melanin.
,
However, few publications exist on this topic and their setups vary widely. Nevertheless, some studies use higher-powered lasers and LEDs, even at half the face, and get great results for melasma. I'm talking about 55-90 mW/cm2+ and 100 J/cm2+ doses here.
I also think that melasma and hyperpigmentation are far more than a "light story" alone - even with ultraviolet light involved. So, that story continuation will be told in the next section!
Next up, there are six light therapy studies for melasma in total. I'll go through these studies one by one:
- First up, a review is exceptionally insightful on light therapy for melasma treatment (90). The good news here is that light therapy can help you treat melasma. Both redness and vascularization can be reduced. Here's what the researchers write:
"Clinical studies, in agreement with in vitro experiments and animal models, suggest that [light therapy] effectively reduces melasma-associated hyperpigmentation. Specific wavelengths (red: 630 nm; amber: 585 and 590 nm; infrared: 830 and 850 nm) at radiant exposures between 1 and 20 J/cm2 exert modulatory effects on tyrosinase activity, gene expression, and protein synthesis of melanocytic pathway components, and thus significantly reduce the melanin content. Additionally, [light therapy] is effective in improving the dermal structure and reducing erythema and neovascularization, features recently identified as pathological components of melasma." (91).
- I'm happy with that finding as it's extremely close to what I found in the previous section. There thus seems to be an overlap in how light affects melanin and how light affects melasma (which I would expect, of course!).
- I'll consider this review in more detail below - after I've checked through the individual studies myself. I don't want to rely on the assessment of the reviewers before I read the individual studies without prejudgment.
- So, first, there's a study using 675 nm for treating facial melasma (92). There were three treatments over three months, with 30 days in between. Participants with Fitzpatrick II and III were included. A laser was used until mild redness and slight edema. Unfortunately, there's not much specific treatment information except that small areas are treated, even in the full text of the study (93). Nevertheless, you can see the improvements of the participants in the table below:
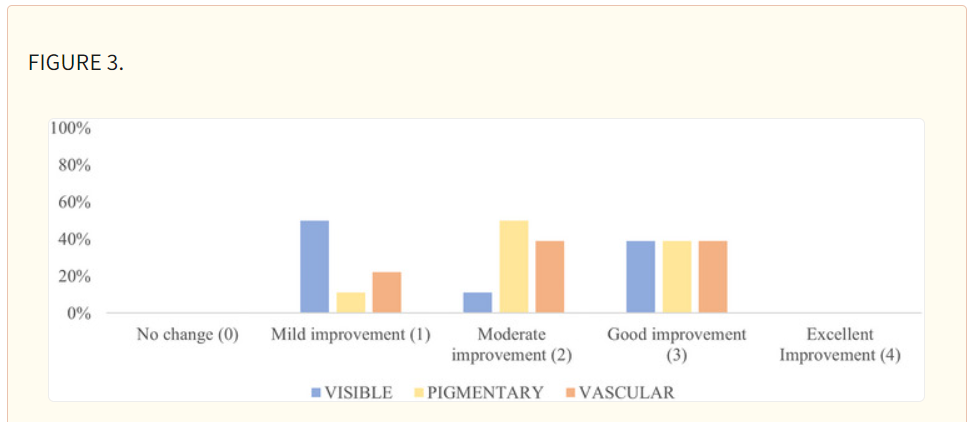
- So, the visibility, pigment, and vascularity of the melasma improved! Here you can see some before and after pictures:
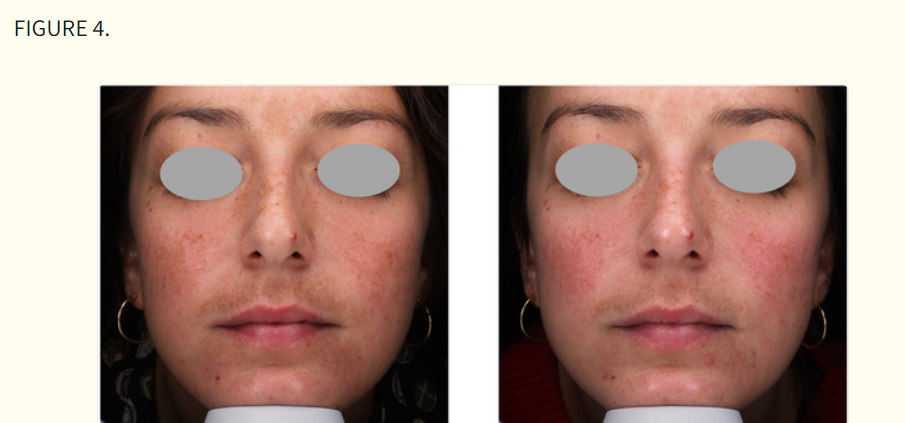

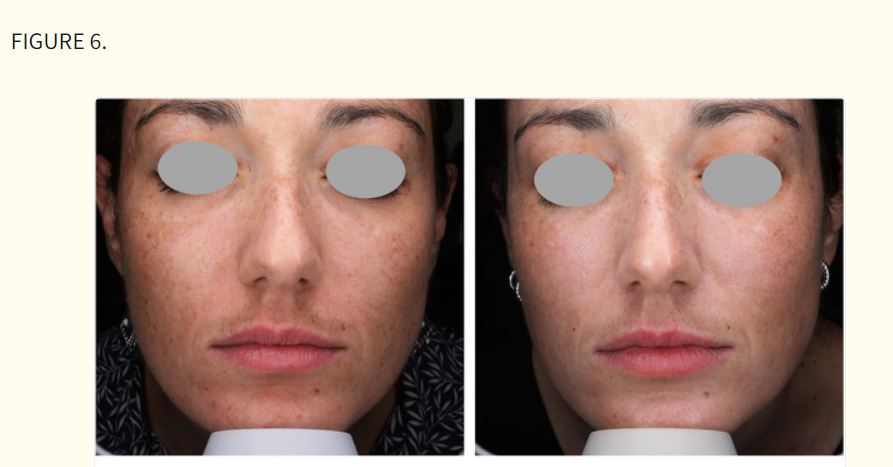
- Some of these pictures are more impressive than others but what's important is that the study participants themselves are generally moderately happy with the results! And that's with three treatments over three months only!
- Pain was well tolerated. Symptoms after treatment were mild (93).
- Given the full protocol mentioned in this publication, however, this However, given the full protocol mentioned in this publication, this seems like a higher-powered laser to remove melasma. That's a remarkable finding but not what you'd expect with light therapy in general!
- Then, there's a 590 nm study using different dosages (94). This is not a study with randomization, unfortunately, so it's impossible to draw certain conclusions about causality (96). The good thing was that the outcome was positive and that 590 nm light inhibited blood vessel growth and melanin formation. The study is quite complex and you may want to read the full text for all details (96). Better studies are needed here, though!
- Then there's a 633 and 830 nm study (95). Fitzpatrick IV and V types are included here. These are 60 female participants aged 25 - 60. These women were split into subgroups according to their Fitzpatrick type. The treatment was 20 minutes. The power output is 55 mW/cm2 for the 633 nm red and 105 mW/cm2 for the 830 nm near-infrared. The total dose comes to a whopping 192 J/cm2! There were 36 treatments over 9 months - about four per month. And, the results were very positive - both assessed by the researchers and the study participants!
- Then, there's one more 940 nm study with a power density of 90 mW/cm2 (96). A total dose of 13.5 J/cm2 was applied. There were a total of eight treatments over eight weeks. Here's the treatment protocol described by the researchers:
"During treatment, the initial mobilization phase with microdermabrasion was closely followed by the modulation phase, delivering low-energy pulsed photons (940nm) to downregulate highly metabolic melanocytes in the dermis. A weekly treatment was performed for eight consecutive weeks." (96).
- Once again, the researchers included tons of measurements for before and after results. Only one side of the body was treated for melasma, while the other was not. Here you can see the percentages of improvement (between 0 and 100%) in the untreated versus the treated side (97):
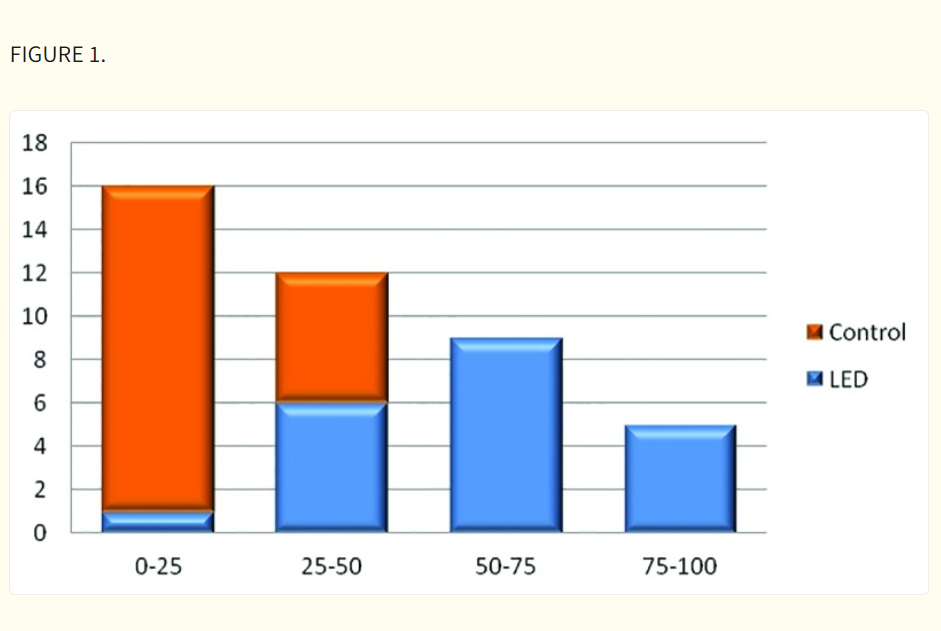
- Next up, you can see the severity of the melasma, also for both sides (97):
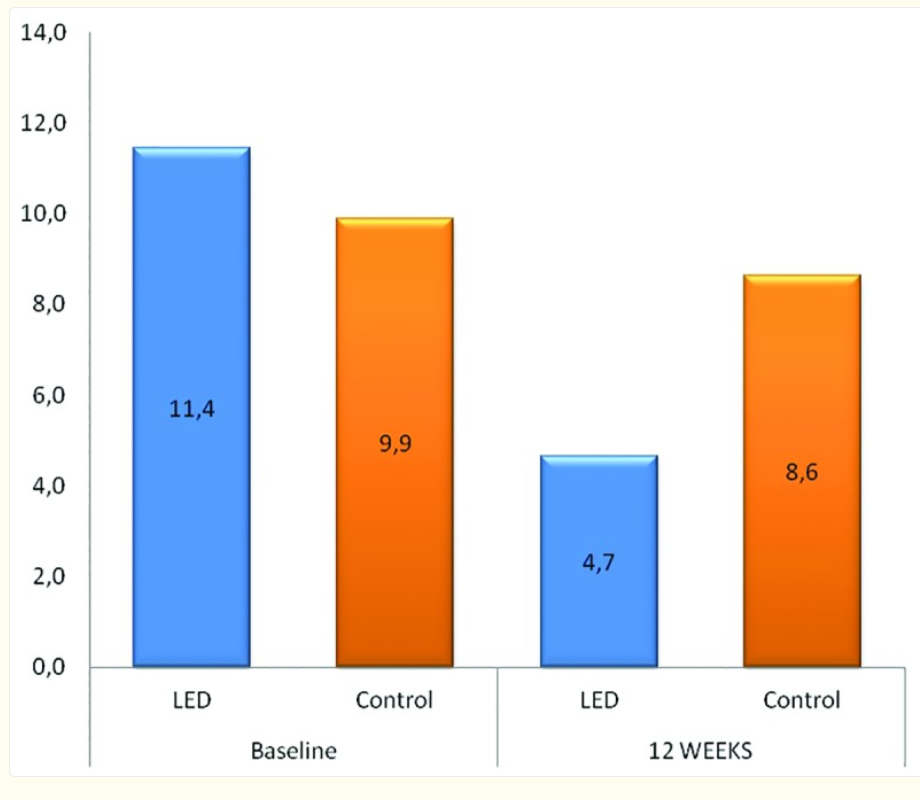
- So the melasma severity, measured with the so-called "MASI score", more than halved! That's fantastic news.
- Next up, there's a picture of the melanin index:
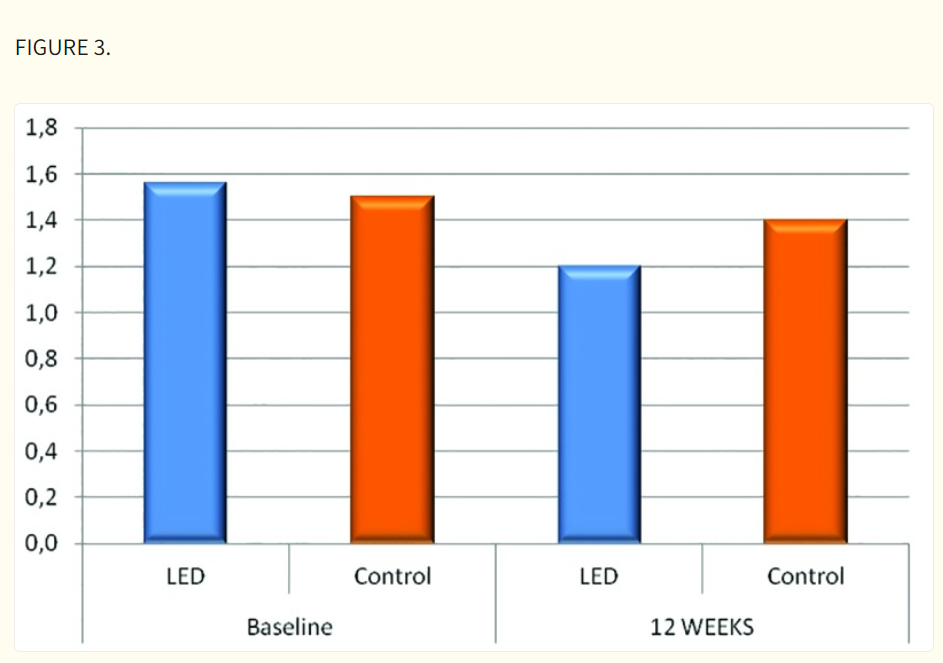
- The melanin index is a scientific measurement of the amount of melanin in the skin - so it's not a rating by the study participants or researchers! There was still an almost 20% decrease here in the treated side although this result isn't as impressive as the previous ones!
- What's interesting here again is the dosing at 90 mW/cm2 - with half of the face treated (12.5cm x 20cm) (97). This dosing protocol, with the considerable improvements in melasma, undermines the common thesis that "high-powered LEDs or lasers" will cause melasma. In this study, the higher-powered application doesn't just cause melasma but actively reverses it!
- The studies I've discussed here are also the only melasma studies out there right now. Again, you can look these studies up yourself by searching for melasma in Vladimir Heiskanen's Excel sheet. If you find studies that I've miseed, please send them to me! You can comment below or reach us in our FB group.
- And, yes, the study isn't anywhere near perfect. It's an Randomized Controlled Trial - the gold standard in medicine - with half the face acting as a placebo and only seven participants (97). I'd like to see far more studies on red light therapy for melasma! Right now, we don't have evidence that high-power exposure of near-infrared even causes melasma, but we have evidence of the opposite effect!
Returning To The Aforementioned Light Therapy For Melasma Review
Let's return to the review I quoted early on (91). I wanted to give this review an independent section because there's so much information. The review also helps me check my conclusions and see where my viewpoints differ from people who have worked on this topic for months and where my viewpoint agrees.
I'll go point by point below:
- So first of all, regarding dosing, I think the 1 - 20 J/cm2 makes tremendous sense, although exceptions exist here as I've mentioned earlier (91). Nevertheless, keep in mind that there are exceptions here, too. These conclusions are based on the human studies, on the in vitro ones! The review does only take three human studies that directly treat melasma into acccount, however! What is interesting is that the review explicitly states the following:
"In light of the necessity of transferring energy from a photon to a chromophore to induce biological activity and cellular processes without incurring thermal tissue damage, light sources in the form of low-power lasers or LEDs (1–500 mW) are commonly employed. Maintaining a low irradiance (<100 mW/cm2) is critical to prevent undesired thermal effects and the initiation of reactions unrelated to PBM." (91).
- One of the studies, however, which they also explicitly quote, uses a far higher power output of 160 mW/cm2 with good results (95). The total dose is also extremely high. I'll return to this topic in more detail at the end of this article. That exposure level probably works because it's still relatively similar to what you'd get on a sunny summer day without clouds, although it does exceed sunlight's maximum dose!
- Secondly, melasma is not just a light story - many other factors are implicated. Examples here are genetics, the medication you take, hormonal dysregulation (a huge problem in modern society), overall blood vessel health, and general inflammation (98; 99; 100)! I'll get back to these later! So, once again, you can't just blame ultraviolet light exposure - melasma specifically and hyperpigmentation in general occur in a broader context of health!
- Yes, it's likely ultraviolet light that loads the bullet to melasma. But, ultraviolet light alone may not pull the trigger! In the same way, movement loads the bullet for knee osteoarthritis, for instance. But it doesn't mean that movement pulls the trigger. And you wouldn't want to tell people to avoid all movement just to avoid getting knee osteoarthritis. In the same way, I'd recommend people still get sensible sunlight exposure (without sunburn) because of the wonderful overall health benefits. Similarly, I'd still recommend people move their bodies despite the risk of getting knee osteoarthritis when they get older! The risk of not moving is too big, because you'll become obese, get diabetes, and may die of heart disease! You'll also massively increase your overall cancer risk. Here's a quote that captures my assessment really well:
"Exposure to UV radiation is a well-known trigger for melasma, as it can induce oxidative stress and promote melanocyte hyperactivity. Furthermore, the involvement of inflammatory mediators, such as cytokines and growth factors, has been implicated in melasma pathogenesis." (91).
- You know what else induces oxidative stress and inflammation? Exercise - temporarily! But you wouldn't want to avoid exercise because it gives you temporary oxidative stress and interrelated inflammation. The oxidative stress and inflammation are even necessary for the beneficial effects of exercise. So if you supplement with antioxidants very close to exercise, you may prevent the beneficial adaptations from occurring in the first place (101; 102; 103).
- The review more or less agrees with me on the best wavelengths - amber at 580 - 590 nm, red at 630 - 660 nm, and infrared between 830 - 940 nm (91).
- You and I do need far more human research on this topic, the few studies available give great insight but there are too many unknowns (91). We need more Randomized Controlled Trials with many participants, who are tested under many different circumstances. With circumstances I mean that participants should be exposed to many different treatment paramaters, such as different wavelengths, high and low power, different Fitzpatrick skin types, including medication or not, correcting for daytime ultraviolet exposure, etc.
- The review more or less agrees with my assessment of the animal studies. They highlight a few mechanisms, such as inhibiting tyrosine activity and thereby melanin synthesis and the recycling of melanocytes. Blue light may be more dangerous, according to the review, which I agree with (91). Again, this doesn't mean you should avoid all blue light in your life - the exposure just needs to be balanced!
- Amber and red light help overall skin health as well (91). Examples here are the better blood flow by red light and the amber light, which prevents, excessive blood vessel creation, which is tied to melasma. Overall inflammation is also reduced.
- The review still focuses on many interventions, such as sunscreens, oral and topical medication (and peels), that I'm not always the biggest fan of due to potential side effects (91). So we disagree here! The review envisions light therapy as one of the tools in a broader toolbox that contains the sunlight avoidance, sunscreen, chemical peels, and so forth!
- Overall, our viewpoints are very similar, especially regarding light therapy!
Next up, let's consider a viewpoint that's just as important as that of light therapy I've considered above:
Artificial Light - Specifically Blue - And Other Factors Causing Hyperpigmentation And Melasma
Modern light environments differ big time from our ancestral ones in that today, there's an overload of blue light and not much balancing red, near-infrared, and ultraviolet light.
That blue light stimulation on the skin and into the eyes may affect the melanin system in the skin. Melanin is present in far more places in our nervous system, such as the brain and the spinal cord.
In this section, I use some of the earlier content of neurosurgeon Dr. Jack Kruse on melanin and melasma. Dr Kruse has convincing arguments that mitochondrial health, your circa 24-hour day and night cycle (the circadian rhythm), and the melanin system are all tied together. Melanin plays a role in immunity, for instance, and has a hormonal function. However, we need far more high-quality studies into this topic before solid conclusions can be drawn!
Nevertheless, there are many other factors affect how well your melanin system functions. Examples here are oral contraceptives for women, nutritional deficiencies, heat exposure (saunas and hot weather), stress, and more.
Light influences human biology across the board. I'd be surprised if (blue) light in our indoor environments and the absence of the natural light we were exposed to ancestrally don't affect the skin as well.
Since 2013, I've been following Dr. Jack Kruse. He's inspired much of my thought on light and health, although I dont't necessarily agree with him on diet and some other topics. For light and its effects on health, Dr. Kruse is brilliant often in my opinion! As he's a polarizing individual for many, just ignore this part of my argument if you don't like him!
Nevertheless, I need to give credit where credit is due! I needed to include this argument because it's vital, in my opinion...
Artificial Light, Hyperpigmentation, And Melasma
Dr Kruse already discussed the strong link between melasma and artificial blue light in 2016 (104). Main topics considered there are hyperpigmentation and melasma, specifically! The thesis here is that if you're in a truly artificial environment that looks nothing like your ancestral environment, there are consequences.
Simply put, light has biological effects. This entire website is dedicated to light's effects on health and helping people supplement their light inputst wherever possible. The truth is that many people can't get sufficient sunlight exposure throughout the day and achieve darkness at night (without the inputs of artificial light).
Hence, you'll have to supplement. As the time-old saying goes, the perfect is the enemy of the good here. Sure, I would have preferred every human on this planet see the morning sunrise and get some afternoon sun for vitamin D and tons of other benefits–but that's life! need to work in an indoors to survive and make money.
So there's not always a choice...
The issue is this: modern light bulbs, screens (phones, tablets, televisions), and many other light sources have peaks around the 400 - 500 nm blue range of the light spectrum. However, sufficient quantities of red light are absent to counterbalance the blue. And, there's no ultraviolet or infrared light emitted by these devices, as they're considered "energy-inefficient".
The key is that modern artificial light doesn't just create mismatches in your circadian rhythm. That circadian rhythm is your human body's circa-24-hour day and night cycle (104). No, the artificial light directly affects the melanin system in the skin.
And, sure, I've often seen the argument stating that "the dose isn't too high" of the artificial light (when you measure it in mW/cm2). That's true, in a sense, but it misses a critical point: there's no natural counterbalance of red, near-infrared, and ultraviolet light.
Kruse often quotes the principle of non-linearity here. That principle simply means that a small stimulus can have a huge effect or that a huge stimulus can have a negligible effect. In other words, there's no linear relationship between the stimulus and response, and a 100% increase or 50% decrease in the stimulus doesn't lead to an equal reaction in the response.
Concerning artificial light, just a tiny amount of blue that stimulates you all day can have a considerable impact. People spend up to 90% of their time indoors nowadays (105; 106; 107). So the indoor environment has replaced our ancestral environment for most humans in the developed world!
But back to Dr. Kruse. The claim is that exposure to artificial blue light can directly lead to hyperpigmentation and melasma over time. But is that thesis true? Let's check some recent studies. Here's the first quote:
"Skin is being increasingly exposed to artificial blue light due to the extensive use of electronic devices. This, together with recent observations reporting that blue light-also known as high-energy visible light-can exert cytotoxic effects associated with oxidative stress and promote hyperpigmentation, has sparked interest in blue light and its potential harmful effects on skin. " (108).
The study highlights how food compounds can counteract the toxic effects of blue light (108; 110). Dietary intake of nutrients may once again be protective against the effects of blue light, in turn (108; 110).
In another study, blue light affected the melanin system in the skin in a dose-dependent fashion (109). Here, researchers write:
"When compared to UVB irradiation, the blue-violet light induced a significantly more pronounced hyperpigmentation that lasted up to 3 months. Histological examination showed a significant increase of keratinocyte necrosis and p53 with UVB, as compared to 415- and 630-nm exposures." (109)
Also, Fitzpatrick type III and higher may be especially prone to the hyperpigmentation effects of blue light (111). Green light may also not be 100% safe and may still be able to stimulate melanin synthesis (112). Even review studies seem to agree with the assessment that blue and green light can harm the melanin system (113; 114).
Remember that I'm not saying that all blue and green light exposure is bad. Instead, I'm claiming that isolated blue and green exposure, without any red or other light naturally present under the sun, is the problem!
And, sure, much more high-quality research is needed here, especially regarding the dose-response relationship. Nevertheless, the data that is currently available is already worrisome and entails me to inform you as the reader about this topic!
Why should you care about this topic?
Well, let's return to Dr. Kruse (104). Kruse highlights Dr. Ignaz Semmelweis and Dr. John Snow, both pioneers in the medical field. These two individuals caused the entire field to rethink its presuppositions. Simmelweis' discovery led to the widespread implementation of hand washing in the 19th Century and John Snow helped mitigate waterborne diseases through sanitation.
Modern society is unthinkable without these!
The same is true in this case if artificial blue light is toxic to modern humans and causes problems down to the hyperpigmentation of the skin level eventually! Sometimes we need a "Copernican Revolution" in medicine to progress!
Detour: Circadian Rhythms And Mitochondria
So, let's talk about the circadian rhythm. I'll later give you the link to hyperpigmentation and melasma. But to do so, I'll have to talk about "mitochondria" first. I've written an extensive article about that topic, which you can read here:
"Mitochondria" are the energy-creating "factories" in your cells–most energy is created there. The current scientific consensus is that ATP - or "Adenosine Tri-Phosphate" - is the primary energy currency created in that cell.
Just like the world still mostly runs on fossil fuels, your mitochondria run on ATP. Some radical thinkers question this thesis, but for now, let's assume it's true.
The problem is that mitochondrial function tends to go down with age. Your mitochondria have their own DNA - that's separate from the DNA in the center of your cell. Over decades, mitochondrial DNA is not everywhere the same anymore - that's called the "heteroplasmy rate".
Quality sleep and a healthy lifestyle keep that heteroplasmy rate down, by the way!
With more divergence in the mitochondria, their energy production goes down. And, if you don't use your mitochondria sufficiently - such as through exercise, cold exposure, saunas, etc - then you'll end up with fewer and smaller mitochondria over time.
The good thing is, red light therapy affects mitochondrial function and boosts their energy production through several mechanisms. Red light therapy has many benefits, such as lowering inflammation, countering oxidative stress, helping you create new mitochondria, and activating parts of genes that support health. The result is improvements in health across the board.
Now, here's the kicker:
There's a super-strong link between your circadian rhythm and mitochondrial function and health (115; 116; 117; 118; 119; 120; 121; 122; 123; 124; 125). Almost every single process in your body is tied to circadian rhythms. And also, almost every single process in your body (if not literally every) is tied to your circadian rhythm.
Here's how your circadian rhythm works: you have a central clock in your brain, in the suprachiasmatic nucleus. That nucleus is affected by the light input into your eye, mainly blue and a little bit of green light. So when blue and green light enter your eyes, it tells the brain it's daytime.
Other factors also tell your body it's daytime, such as exercise, your food intake, cold exposure, and so forth - but light is the most important one!
If that light input into your eyes is incorrect, different modern diseases will eventually arrive. Whether it's heart disease or cancer or diabetes or neurodgenerative disease, all are linked to circadian rhythm disruptions. And with circadian rhythm disruptions, mitochondrial function also goes down, further increasing disease risk.
The problem here is the omnipresent artificial blue light in modern society. Artificial blue (and, to a lesser extent, green) tell your body it's daytime. But, if you're exposed to screens and blue LEDs at 11 PM, a few hours after sunset, that creates a huge mismatch. Your body thinks the sun has just come up, even though it's night. And, the circa-24-hour circadian rhythm clock is totally thrown off.
Essentially, you're creating mini-jetlags or mini-night shift work sessions. And, such disruptions have a huge impact on your overall health - you can find tons of great recent reviews on this topic (126; 127; 128; 129; 130; 131; 132; 133; 134; 135; 136). It's not just that you feel bad on a jetlag or doing shift work–it's that your body takes a substantial hit at the fundamental level each time you engage in that bevavior.
Could the skin be the only system not affected by circadian disruptions? Let's explore:
Circadian Rhythm, Hyperpigmentation And Melasma
So, I've established that almost any bodily system is linked to your circadian rhythm. Would it be likely that the melanin system in your body, such as its primary cells, the "melanocytes", are also affected by the circadian rhythm?
Bingo!
For nerds, here's a fantastic quote - that's quite long - from a recent review on the topic:
"Melanocytes produce melanin to protect the skin from UV-B radiation. Notwithstanding, the spectrum of their functions extends far beyond their well-known role as melanin production factories. Melanocytes have been considered as sensory and computational cells. The neurotransmitters, neuropeptides, and other hormones produced by melanocytes make them part of the skin's well-orchestrated and complex neuroendocrine network, counteracting environmental stressors. Melanocytes can also actively mediate the epidermal immune response. Melanocytes are equipped with ectopic sensory systems similar to the eye and nose and can sense light and odor. The ubiquitous inner circadian rhythm controls the body's basic physiological processes. Light not only affects skin photoaging, but also regulates inner circadian rhythms and communicates with the local neuroendocrine system. Do melanocytes "see" light and play a unique role in photoentrainment of the local circadian clock system? Why, then, are melanocytes responsible for so many mysterious functions? Do these complex functional devices work to maintain homeostasis locally and throughout the body? In addition, melanocytes have also been shown to be localized in internal sites such as the inner ear, brain, and heart, locations not stimulated by sunlight. Thus, what can the observation of extracutaneous melanocytes tell us about the "secret identity" of melanocytes?" (137)
I'm the first to admit that a lot more research is needed here. But the melanin system in your body is far more than just protection against ultraviolet light. Melanocytes have a hormonal and immune function. The melanocytes also participate in the circadian rhythm. So, the melanocytes are a mechanism through which light, as an input from the outside world, can be translated into a message and energy into the body.
Again, much more research is needed in this area. Nevertheless, the implications for human biology are gigantic. Here's a display of the role of melanocytes in human biology according to the paper I just quoted (138):
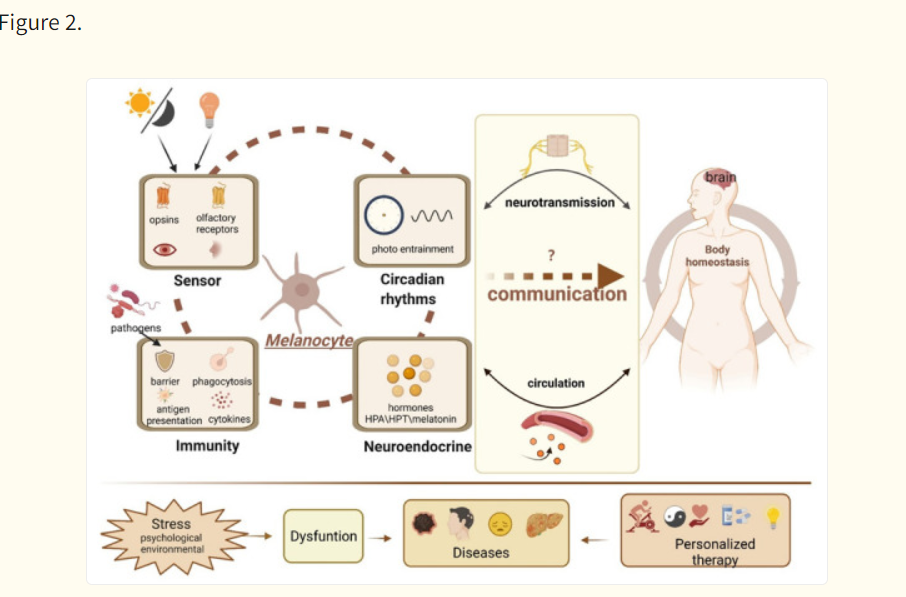
These melanocytes also play a role in the periperhal circadian rhythm. You see, the peripheral circadian rhythm - small "clocks" in all your cells - needs the central clock of the suprachiasmatic nucleus that I talked about before.
This dynamic has been understood as that of a conductor with its orchestra (139). If the timing of the conductor or the orchestra is off, the music will be horrible. You will only end up with beautiful music by strict coordination of the orchestra and conductor. It's the same story with the peripheral clocks in your cells and the central clock in your brain!
Thowring off the central clock through light at night, or strong stimulation of the skin during the night, thus leads to unwanted consequences. You'll want darkness at night and the (correct) light input during the day.
Here's what the same review I quoted just before states about the dynamic of the melanocytes and the central clock in your brain:
"However, critical questions as to why melanocytes are equipped with so many functional devices and to what extent these physiological functions can be exerted and even whether there is coordination between these functions, such as neuroendocrine activities and circadian rhythms, should be further integrated. Despite how these activities affect local physiology, how they transmit and amplify signals and even integrate with other remote tissues remains relatively unknown. Undoubtedly, the numerous activities of melanocytes are complex and highly controlled processes. Therefore, deciphering the mechanisms of the communication process can potentially contribute to gaining insight into the pleiotropic roles of melanocytes within the organism and can open a completely new horizon for revolutionizing the way diseases will be diagnosed and treated in the future." (138)
So, it's highly likely that this connection between the circadian rhythm and the melanin system exists–the mechanisms are just not understood well. And melanin isn't just found in your skin but also in your eye (140). That's a whole other rabbit hole we could go down to but won't today. That eye is the strongest link to your circadian rhythm.
Melanin is also found throughout your nervous system in the form of "neuromelanin" (141; 142; 143). Both share the same pathways in that they're derived from the protein building block ("amino acid") tyrosine, and related to dopamine (which aids motivation and abstract thought). So melanin seems to be present in more and more places throughut the body, not just the skin!
Suffice it to say there's an ever stronger link between the circadian rhythm, light exposure, and melanin. Yes, as stated before, this topic needs to be researched a lot more in high-quality human trials (insofar possible!).
But the links are all there: that of circadian rhythm disruptions and related changes in the melanin system. The simple truth here is that most of us aren't exposed to the light environment your ancestors grew up in. Your ancestors only moved indoors in the early 20th Century, when most people left agriculture in the developed world. And with that move, there's likely an insurmountable impact on the melanin system that's yet to be fully understood!
But for me, it's very hard to just blame ultraviolet light exposure or red or near-infared light. Those conclusions may sound simple and give the false appearance of knowledge–but they won't help the average person!
Let's take another step back:
Dr. Kruse On Melanin And Health
Lastly, I want to explore some of Dr Jack Kruse's latest thoughts on melanin from 2023 and 2024. Those interviews are mainly important if you're interested in the topic from a scientific standpoint - they will be very hard to follow for the average person.
(Don't worry I've added a summary below!)
You can check the three interviews - the first two with Andrew Huberman - below, beginning with part I:
Then there's part II:
And, finally, part III:
If you want the short version of Dr Kruse's argument, here they are. First part I:
- Light, water, and magnetism rule human biology from a physics perspective. Dr Kruse found out about those when he lost his health, earlier on. He changed his paradigm (simplified: an overall viewpoint on a science) and healed himself. The key here is that melanin runs throughout the entire human body, as we've recently seen in the science, and is much more important than mainstream medicine currently suggests. So, the viewpoint of "melanin" for just ultraviolet light protection is completely wrong. Our melanin system is far different from primates' because we lost most of our bodily hair. Humans also evolved around the equator, where sunlight was available year-round. The human body is like a semiconductor, in that its proteins and the water content work together to capture light energy from the environment. That light energy is precisely what has been lacking in the last century or so, for most people. Light influences the production of melanin not only in the skin but also throughout the body and is vital for the circadian rhythm.
Additions in part II:
- Water plays a significant role in the health of the cells and everything outside cells, the energy creation process, and more, in that the water itself can change structure. Dr Kruse is a proponent of Deuterium-depleted water (especially if you're in poor health). We're also back at melanin's role in health here, which is creating energy and helping motor functions. Modern medicine has the current flaw that it doesn't focus much on the physics perspective on health, even though many implications could be deduced from physics laws on the human body.
Lastly, part III:
- This third episode also considers the role of melanin - precisely that it can capture all frequencies of light - according to Dr Kruse. I've also quoted the studies that Dr Kruse focuses on earlier, the neuromelanin that's found in the nervous system and implicated in neurodegenerative disease once it's gone. A specific area in the brain, the "substantia nigra" - whereby the "nigra" signifies the darkness of this area because of the high melanin content - degenerates during Parkinson's Disease.
So, potentially, the melanin system plays a much bigger role in health than is commonly appreciated! Avoiding all ultraviolet light is thus not recommended in my opinion. Fortunately, sunlight is getting a re-evaluation right now with many recent studies showing a big increase in how sunlight exposure is valued for health and preventing disease!
Lastly, I want to consider a few other reasons for hyperpigmentation and melasma that Dr. Kruse already laid out years ago:
Other Factors Influencing Hyperpigmentation And Melasma
Here are a few other reasons for hyperpigmentation and melasma that few people think about:
- Oral contraceptives seem to increase the risk of melasma massively - this fact has been known since the 1960s already (144). The same is true for pregnancy, as already stated in an earlier section. I'm really sorry, women! I wish things were different here...
- Oral contraceptives change hormone levels such as progesterone and estrogen, thereby increasing hyperpigmentation risk (145; 146; 147; 148; 149). I was surprised that there's not much more high-quality research available on this topic, as you'd expect that women would really like to be informed about this topic! You can even fix the melasma sometimes by switching contraceptive methods (149). Given that so many women use oral contraceptives, and the link to melasma, there should be far more research in this area!
- What's surprising - or maybe not - is that women are also most often affected by hyperpigementation and not men (91). I wonder whether the link between oral contraceptives and hyperpigmentation decreases that difference, although there are more differences.
- Estrogen increases melanin production, for instance, and is also affected by oral contraceptives. Progesterone also influences melanin levels, although this mechanism is less well validated.
- The effect of oral contraceptives is the strongest for darker skin types or those already predisposed to melasma or hyperpigmentation.
- These hormonal changes, due to contraceptives, may also change your tolerance of ultraviolet light (150; 151; 152; 153). And we've returned full circle, with that claim!
- Here's what one study writes about the dynamics I've described above:
"The most common time of [melasma] onset was after pregnancy (42%), often years after the last pregnancy, with 29% appearing pre-pregnancy and 26% during pregnancy.
[...]
"The odds of melasma occurring for the first time during a pregnancy were also increased with multiple pregnancies (twice the odds if 2 vs. 1 pregnancies, three times higher if 3 or more vs. 1 pregnancy). Of the women, 25% who had used hormonal contraception claimed that melasma appeared for the first time after its use, the rate being higher for those without vs. with a family history." (150)
- Again, I'm very sorry for my female counterparts!
- It's also known that oral contraceptives can directly change skin physiology (154; 155; 156; 157). Inflammation in the skin changes, for instance, potentially leading to a different response to ultraviolet and blue light that you would have otherwise not seen.
- Please keep in mind that I'm not saying never to use oral contraceptives! Instead, you should be aware of the potential downsides, especially for melasma and hyperpigmentation!
- Other reasons why you may end up with hyperpigmentation are also postulated. In his Time 20 blog, Dr Kruse talks about why grounding is essential to health in combination with a natural light spectrum (158). Grounding or better yet, Earthing - whereby your feet touch the sand or grass or another conductive material - helps blood flow and lowers overall inflammation. Dr Kruse also posits that the water in your body changes to EZ water - although that statement is more questioned in the current scientific consensus. EZ water holds charge and boosts energy efficiency of the body. Mitochondria are also strongly affected by the light in your environment - which you probably know about because you read an article about red light therapy. The overaarching message here is that with a very different light environment and lifestyle, modern humans have removed themselves from their evolutionary past. The way your ancestors and mine interacted with light for millions of years has changed since the Industrial Revolution and modern electricity. Earthing likely also changes the way light interacts with your body - because of the changes in water structure!
- You'll at least have to be aware of that dynamic, although I'd love to have seen many more studies that compare a modern indoor light input with a more outdoor option - but these studies are prohibitively expensive to carry out, especially if you have to run these studies for years or even decades to find long-term effects!
- On this topic of environment, Dr Kruse writes the following in a Facebook post:
"The skin acts not only as a target for neuroendocrine signals but also a source of hormones and neurotransmitters, particularly the epidermis. Melasma is an uneven type of pigmentation of the skin of women when they lose the ability to fat burn in their mitochondria. Recent studies have shown that 470 nm light is especially capable of causing melanogenesis especially when UV and IR light is subtracted. Some of the reasons are discussed in this blog [Time 20]. One that is not is that 850 and 870 nm light have been shown to decrease melanin ability to made to limit the effect of pigmentation in vitro. That is [near-infra]red light. 470 nm light is in the blue color frequency and has been shown in many new studies that unevenly cause pigmentation. All technology LED displays release that light. So the more selfies you take the more uneven pigmentation you should expect. Mitochondrial biology is amazing when you understand it." (159).
- Blue light overexposure and an unnatural light environment, are what cause that loss of fat-burning capacity in the mitochondria (160).
- One of the key mechanisms through which oral contraceptives affect skin health is through nutrient depletion. These effects have been well established since decades but I don't see many people talking about the topic (161; 162; 163; 164 How strong these effects are, we still don't have great research about (at least high-quality). However, an effect certainly seems to exist and needs to be taken into account. Again, I'd like to have better data on this topic! It's crazy to me that this topic hasn't been studied in much more detail!
- Gut issues are likely linked to hyperpigmentation and melasma (and skin health in general) (165; 166). Much more research is needed here though!
- PUFAs (anecdotally). These are the traditional "seed oil" or "vegetable oils" - many people using them report their sunlight tolerance is much better once they switch to other fats, such as (extra virgin) coconut oil, extra virgin olive oil, butter, tallow, ghee, and other natural fat sources. PUFA-rich (omega-6 rich) oils have never been consumed in large quantities in human history.
- Heat exposure - although you'd need to go very far here and usually this is not the case with red light therapy, as there will be minimal skin warming even with high-powered panels. Cooking fire is linked to melasma risk, for instance (167). The effect of heat on the melanin system is shown in different studies (168). My argument here is that if you're afraid of heat causing melasma or hyperpigmentation, you should avoid tropical and subtropical destinations for your holidays. And, stay indoors when it's hot outside. Avoid any saunas because they heat up the skin quickly. The irrational thing to do would be to avoid red light therapy panels, even full body panels - as these heat up the skin far less than being outdoors on a sunny day or with a sauna! And if you're afraid of panels overheating you, just use your panels in a cold room - the problem should be solved then!
- Stress and anxiety - can change the melanin system in the skin, believe it or not!
- Medications can change the melanin system, such as with photosensitizers. So beware here, especially if you're taking something long term.
The moral of this section?
Hyperpigmentation is much more complicated than avoiding ultraviolet light at all costs. There's an intricate dynamic regarding the correct light exposure and skin health and function. And many factors play a role here, not just the light in your environment, even though that may be the first domain everyone starts looking at!
Conclusion: Welcome To The Melanin, Hyperpigmentation, And Melasma Revolution!
I'm very sorry that I can't give you a simple answer. The most straightforward "way out" for me would have been just to blame ultraviolet light, or indoor blue light, or high-energy red light - but that's not the case in any of the examples I've given above!
The human body is a complex system. Your nutrient intake certainly plays a major role in your skin health, as well as your circadian rhythm, as well as your mitochondrial function, as well as the light you exposure yourself to during the day, as well as the absence of light (hopefully!) at night, and so forth!
I wish I could pinpoint a single reason, but I'd be oversimplifying!
And, my findings are far from perfect! As stated in the article above, far more high-quality human studies are needed on both hyperpigmentation and melasma in relation to light therapy! We also need more studies on the curative effects of light therapy - such as using high-powered lasers locally on areas with melasma or hyperpigmentation to normalize the skin.
And, many other questions give limitations to this article:
- What's the exact effect of each of the factors influencing your hyperpigmentation or melasma risk, such as light input, genetics, diet, sleep and circadian rhythm, and more?
- Even if there are short-term studies, what are the long-term effects of all these inputs?
- What is the exact relationship between sunlight and red light therapy? Do you even need red light therapy with sensible sunlight exposure?
- Can red light therapy be misused and lead to side effects? So, some of the studies use higher-powered red and near-infrared light to remove melasma - but would new studies show (potential) side effects here?
- What are the best dosing parameters for red light therapy for melasma and hyperpigmentation? The way studies are currently set up, you'd need at least dozens of human studies that test different power outputs, pulsing settings, wavelengths, Fitzpatrick skin types, and so forth!
So for now you and I need a multi-dimensional and multi-factorial approach to hyperpigentation. Nevertheless, if you implement all of these strategies, especially for preventive purposes, it should already be a game-changer for your melasma and hyperpigmentation risk. I don't say that there are any easy answers. But, you can start with:
- Eating a healthy diet
- Minding your circadian rhythm
- Getting great quality sleep
- Exposing your skin to the morning and midday sun, but not too much and not too little!
- Be careful with medication and oral contraceptives
- Avoid blue-light rich environments if possible!
Let's marry the ancient wisdom of the natural environment of our ancestors, with cutting-edge modern day science - for the best outcomes!
This is a post by Bart Wolbers. Bart finished degrees in Physical Therapy (B), Philosophy (BA and MA), Philosophy of Science and Technology (MS - with distinction), and Clinical Health Science (MS), has had training in functional medicine, and is currently chief science writer at Lighttherapyinsiders.com
Found This Interesting? Then You Might Like:
- Start Here - Light Therapy 101 & Buyers Guide
- What Is Red Light Therapy?
- Discount Codes, Deals & Recommendations - Red Light Therapy
- The Red Light Therapy Facial Fat Loss Link: Myth Or Reality?
- Red Light Therapy For Face Before And After: Unbelievable Results!
- Red Light Therapy For Sunburn: Prevention and Treatment
- Red Light Therapy For Skin: Beauty Benefits, Potential Complications, And More
- Does Red Light Therapy Help Scars? The Science,