This blog post is part of a long series on red light therapy and dental health. This first installment is about dentin hypersensitivity, because it's a very common complaint of people.
Also, very often many people have great results with red light therapy for dentin hypersensitivity. Our very own Alex Fergus even describes that in his dentist experience.
Below, I'll explain to you how red light therapy can help here, step by step!
This article is part of a more comprehensive series on red light therapy for dental health. My first blog focuses on dentin hypersensitivity, one of the most frequent complaints in dental practices. It is characterized by sharp pain triggered by stimuli such as hot or cold temperatures or pressure due to exposure to the dentin, the layer beneath the tooth enamel. The enamel is the hard outer layer of the teeth, affected when you have caries.
Different causes of dentin hypersensitivity exist, but these are not fully understood. Two common causes are enamel wear and gum recession. Fluid movements within the microscopic tubules in the dentin are the dominant theory of why dentin hypersensitivity happens. These tubules transmit sensory information, and when disrupted, they cause heightened sensitivity.
The conventional treatment option for dentin hypersensitivity is fluoride treatment, specialized toothpaste, or numbing treatments at the dentist. All these treatments probably have side effects from a holistic health point of view (I know, an overused term, "holistic"!). Two more problems are that hypersensitivity is hard to diagnose and that dentist don't treat the condition without the patient asking, most of the time.
Fortunately, many randomized controlled trials on red light therapy for dentin hypersensitivity exist. Most of these studies use red and near-infrared light with almost universally positive outcomes! Generally, the effects of red light therapy are as good as numbing agents and fluoride treatments, and often work even better. Combining these strategies works even better, but compounds like fluoride in the mouth (an area that absorbs substances really well) isn't safe.
The most frequently used wavelengths were 630 nm, 650 - 660 nm, 808/810 nm, and 1,074nm. Generally, total doses from 2-10 J/cm2 seem to work best. I recommend you start conservatively and go from there, adjusting by trial and error and always monitoring your outcome. None of what I write is medical advice, so consult with your dentist first!
In most studies, high-powered lasers apply light to either the teeth or the gingival tissue around the teeth (thereby penetrating the light to the tooth's root) for a short time. There's way more detail and context related to these topics, so read the full article below if you want to know the whole story.
Red light therapy for dentin hypersensitivity provides short, medium, and long-term benefits, for periods of up to months. Often, study participants have 40-70% pain reductions, that last for months in not just one but many studies.
These effects are achieved by changing neuronal function and reducing inflammation in the interrelated dentin and pulp area. That pulp lies beneath the dentin and when it is affected, you will almost certainly feel pain. Then there's the stimulation of blood flow and tissue repair in the dentin area. Over time, you may get a deposition of secondary dentin, which reduces dentin permeability and, consequently, pain. However, all scientists do not yet agree about these mechanisms and even the explanations of what causes dentin hypersensitivity!
For the best results, I recommend you visit a dental clinic that applied red light therapy, because they have extensive experience guiding patients. For home treatment, I currently recommend the LightpathLED Diesel Torch (code ALEX saves) because you can treat individual teeth at high power, in a way that comes close to what the study setups use. For full dosing guidelines, read the article below!
Lastly, please don't forget about the many nutrition and lifestyle changes that can help manage hypersensitivity. Examples here are proper oral hygiene, dietary habits, and the use of hydroxyapatite toothpaste, which can help repair dentin. Hydroxyapatite, a naturally occurring calcium-phosphate compound that makes up the tooth’s enamel, has been shown to occlude dentin tubules and reduce sensitivity over time, often outperforming traditional desensitizing toothpastes.
What Is Dentin Hypersensitivity And What Are Its Causes?
So there's a problem: Dentin hypersensitivity is one of the most common complaints that people have for the dentist (1). But currently, there's no universally accepted guideline on how to deal with the problem.
So let's start with the basics:
(Please note that I'm quoting the most recent research on this topic, so from the last 5 years, for my overview on dentin hypersensitivity)
The enamel is the outer structure of the teeth, that will be first affected if you have caries. The dentin is the tooth's middle layer. So your dentin is located below your enamel. That dentin can get "hypersensitive", meaning that you're more sensitive to pain, from hot or cold or pressure.
And under the enamel and dentin, you'll find the dental pulp, where nerves and blood vessels are located. Once caries have penetrated into the pulp, you'll often be "surprised" by the characteristic shooting pain. But, dentin itself can also be sensitive, leading to dentin hypersensitivity.
Penetration of enamel isn't the only reason you can have dentin hypersensitivity. If you love the gingival tissue, which is the "pink skin" on the bottom of your teeth towards the jaw, you can also develop dentin hypersensitivity.
The most commonly accepted cause of dentin hypersensitivity are fluid movements in the dentin tubules. These tubules have microscopic tubes that is calcified. These dentin tubules are responsible for transmission of sensory information, such as hot or coldness, pressure, and also chemical info. As a result, normally, the body can initiate repair mechanisms once damage is done.
That's why many biological dentists that I either know or follow, think that both the enamel and the dentin can be repaired. Some of the best biological dentists I have already followed for some time are:
- The Gator Dentist on X - who informed me about many basics of dentistry, introduced me to hydroxyapatite, a great ingredient for revering early cavities, mouth breathing and oral health, and tought me a ton about proper dental care and what to look out for in a dentist.
- Dr Dominic Nischwitz - who taught me a lot about the dangers of root canals, the potential dangers of titanium implants and why ceramic is better, and, a lot about general oral health practices.
- Dr Weston A. Price - , he doesnt' really need a mention, but for the people who don't know him, he's extensively described the role of diet, especially fat-soluble vitamins such as A, D, E, and K2, and minerals such as calcium, phosphorus, and magnesium, for oral health. Also, Price described the first dangers of the diets in the developed world, with the reliance on tons of grains, which are foundationally different from our human ancestral diet. It's a disgrace that these facts aren't commonly known today, almost 80 years later.
- Dr Mike Mew - who popularized and has a great explanation about the evolutionary mechanism of proper jaw and teeth development. In essence, your teeth and jaw need to experience pressure and that pressure has been largely removed from the modern diet in the "developed world". Without chewing on harder food during your childhood and adolescence, your teeth won't develop properly.
Holistic oral care, such as getting rid of dangerous root canals, check up on any dental implants you have, optimizing your nutrition in a way that works for you, avoiding mouth breathing at all costs unless you perform at above your 90% max heart rate, the ability to remineralize teeth with natural toothpaste (such as with calcium carbonate and hydroxyapatite), avoiding toxins in many different dental products, and more.
But back to dentin hypersensitivity. Here are the current theories on this topic (2). Besides the hydrodynamic theory with the dental tubules I talked about before, the dentin may be directly "innvervated" - so may have sensory neurons at the very least (2). There may also be a sensitization process, whereby the pain process in the nervous system gets altered. The odontoblasts, which create the dentin, may also have sensation itself. And, a concept called "algoneurons" may play a role in this dynamic, which implies that the whole sensory and pain system works very differently in the teeth than in the rest of the body (3). The entire process of how dentin hypersensitivity originates in relation to pain and the nervous system isn't fully understood yet (16).
Also, dentin hypersensitivity is just painful but lowers quality of life (4). The most affected teeth are located at the front of the lower teeth, and the premolars at the 45-degree angle of the lower teeth. Women and those of 20-40 year of age were more often affected (4; 14).
People with hypomineralization of the premolars and molars, which are the teeth located towards the back, also have dentin hypersensitivity more frequently (5). This topic relates to Dr Weston A Price's work, which considers mineral and fat-soluble intake the most essential nutrients for maintaining proper teeth mineralization.
Of course, you should also use common sense - such as not using acidic citrus fruits or lots of ice throughout the day, which can cause dentin hypersensitivity. Or, instead, if you have gum issues and don't treat them for very long, while you have recession in the gums, you'll also eventually end up with problems.
Also, one in ten people worldwide is currently affected by dentin hypersensitivity (15). There's also no good prevention that universally works yet (16). And, just as importantly, often, the diagnosis of dentin hypersensitivity relies on patients themselves - the diagnosis is not often part of routine checkups, unlike the gum tissue or caries/cavities (16).
Nevertheless, once you get a diagnosis, let's explore what your options are:
Current Dentin Hypersensitivity Treatment Options
Desensitization is a common treatment option for dentin hypersensitivity (1). But, the long-term implications aren't well known of that practice. Here's a description of how dentin hypersensitivity is often diagnosed treated in the USA by dentists:
"The majority diagnosed DH with patient self-reporting, confirmed by exams (81.8%), applying air blasts (53.7%), or cold-water (52.3%). They treated patients with DH often/very often with over-the-counter desensitizing agents (90%), and prescribing fluoride formulations toothpaste (82.8%) and/or potassium nitrate toothpastes (60.9%). In their offices, the majority (73.2%) educated their patients often/very often about DH and used fluoride dental varnish for treating DH (71.8%)." (5).
So, air blasts, cold water, and an exan is applied to provoke pain. And when there's pain, fluoride toothpaste or potassium nitrate toothpaste (a desensitizer) are prescribed. The problem here is also that dentin hypersensitivity is hard to diagnose - because you may have a problem in the dental pulp causing the pain, or a cracked tooth, or gingivitis (gum inflammation), or another issue that explains the same symptoms (13).
Nevertheless, as is almost always the case in healthcare, factors are multifactorial. Here are other modalities that may need to be dealt with in dentin hypersensitivity:
"There are several risk factors for [dentin hypersensitivity], including loss of tooth structure by erosion, attrition, abrasion or abfraction, bruxism, gingival recession, occlusal trauma, and abnormal tooth position. These risk factors, in turn, are closely linked to the patient’s dietary habits, such as frequent consumption of fruit juice, soft drinks, and alcohol, and tooth brushing habits, which include method of tooth brushing, type of toothbrush and toothpaste, and frequency of tooth brushing" (16).
Many of these options will need (immediate) treatment by a dentist, such as advanced-stage bruxism (teeth grinding), abnormal tooth position in adulthood, or gingival recession that cannot be reversed. Not treating these will cause problems - and I wouldn't rely on red light therapy alone here - a topic which I'll come to later.
Other common treatment options for the earlier stages of dentin hypersensitivity do work, such as fluoride or gluma (which block the dentin tubules (6). But, I'm worried about side effects here, because I know for sure that fluoride does have side effects which can be horrendous even (7; 8; 9; 10; 11; 12). When compounds are very highly absorbed through the mouth, why take the risk of brushing your teeth with it every day, especially if better non-toxic alternatives are available?
So, with that being said, let's explore how light therapy can help with dentin hypersensitivity:
How Light Therapy Helps With Dentin Hypersensitivity
Next up, I'll cover how light therapy helps with dentin hypersensitivity. To accomplish this, I've used Vladimir Heiskanen's epic datasheet with red light therapy studies.
My Methodology For This Section
I didn't cherry-pick studies during this process. So if there are 40 studies available on red light therapy for dentin hypersensitivity, I've included all 40 of them. I didn't just use four studies randomly in order to write an article, which is, in my opinion, scientific malpractice.
Having said that, I will fully admit that my process isn't perfect either. In a perfect world, I'd have unlimited funds and could do a lot of extra analysis for each article, such as rating it on the bias, pooling the data and statistical outcomes of many of these studies, etc. But, our company is not taxpayer funded, so such time-consuming projects aren't possible right now!
What Study Setups Look Like
Many of these studies use dental hypersensitivity testing, such as a cold stimulus, or evaporation of hot water from a syringe, or electrical stimulation, and then monitor the reaction of the patient/study participant.
Often, participants have to disclose a Visual Analogue Scale (VAS) scale that measures pain from a scale from 0-10. Here, "0" stands for "no pain", and "10" means that you're having the "worst pain imaginable". The outcomes of the VAS scale are then statistically compared to see whether a statistically significant difference can be measured.
If you measure a statistically significant difference, you know that your intervention treatment works better than placebo.
Human Randomized Controlled Trials - Which Have A Very High Level Of Evidence
So here I'll explore the "Randomized Controlled Trials" (RCTs) on dental hypersensitivity. The basic idea of an RCT is that there's an intervention group and a control group. That way you correct for the placebo effect, whereby the beliefs of study participants in a treatment can make the treatment work better.
So, if you think a pill is working even though it just contains a negligible amount of sugar, the pill will have a biological effect because of your beliefs. To correct for that effect and understand the true results of the treatment, the effects of the placebo group and intervention groups are compared.
So here are the randomized controlled trials on dentin hypersensitivity:
- In the first study I'll consider, patients were included that had teeth sensitivity close to the gums (34). There are four groups: 1) laser stimulation (which seems like control?), 445 nm blue light, 660 nm red light, and 970 nm near-infrared light. Sensitivity to cold was measured over time up until a 6-month period. The sensitive parts of the teeth near the gums didn't have caries but participants did get composite restoration, meaning that dental filling was added. The whole study setup was a bit more complicated than I'm describing here but I'll give you the basics. The light was applied to the sensitive area. Light at 660 nm and 970 nm led to improvements in dentin sensitivity from the 14-day mark up to six months. Blue light at 445 nm only worked after 3 months but still had an effect. The light was applied before the participants underwent dental restoration. The structure of the dental tubules also improved!
- Next up, a study of 970 nm applied to participants who were periodontally compromised (35). Hypersensitive teeth on one side of the mouth received a placebo treatment while the other didn't. After three months, the pain in the laser treatment part of the mouth significantly decreased.
- Then, 808 nm light was compared to nitrate potassium (a numbing agent) or both (36). After one and three months, there was no difference in pain between the groups. The positive thing there is that near-infrared light can help as well as a numbing agent!
- Next up, 660 and 810 nm light, with either low power or high power, were compared to fluoride and a placebo laser after periodontal surgery (37). Dentin hypersensitivity was reduced in all three treatment groups but after a week the higher-powered laser worked best. That's great news, as it's another reason we can avoid fluoride in the mouth!
- One more study investigated the effects of the teeth structure close to the gums, at 60 J/cm2 and 808 nm light (38). The control group received potassium oxalate gel. After four treatments, the high-powered laser group had similar effects to the gel treatment, in terms of pain reductions. A lower-powered laser worked less well.
- Then, a study combines nano-hydroxyapatite gel and different lasers (39). One of the lasers here, the GnHAP laser, emits nano-hydroxyapatite even. All groups showed improvement but the GnHAP laser worked best!
- Next up, a study using 660 nm toothbrush that emits 6 J/cm2 as a total dose (40)! Three groups were used: 1) fluoride; 2) red light therapy; 3) both fluoride and red light therapy. The combination of red light therapy and fluoride worked best, but just red light therapy also worked for hypersensitivity!
- One more study shows that a combination of red light therapy and a desensitizing agent works better than either alone (41). Light was emitted at 810 nm. But, statistical significance was only reached after 12 weeks, so that light therapy alone or the desensitizing agents would work well earlier on also.
- Another very interesting study compared a calcium-phosophate-fluoride combination with red light therapy (42). Combining these two works best, but, red light therapy alone also showed improvement.
- Then, a fascinating study where 1,064 nm outperformed 810 nm after three and six months (43). Both groups experienced benefits in hypersensitivity though, after one treatment already. But after three and six months, the results with 1,064 nm were better.
- Furthermore, a 904 nm laser was compared to a desensitizing agent (44). After one week and after three months, the laser outperformed the desensitizing agent, but not immediately.
- Next up, a study using the Thor Photomedicine device during deep cleaning of gum tissue (45). Here, tartar is removed from the teeth and the tooth is smoothened - even below the gumline - to reduce inflammation and allow the gums to reattach. A 10.4J/cm2 dose at 174 mW/cm2 was applied at 660 nm. Even after 2 minutes, the 660 nm laser outperformed the control. The participants had two teeth treated with the laser and two teeth got a control treatment with just one treatment. The improvement lasted up to two months. Here's a demonstration of just how insane these improvements are to tactile stimuli (46):
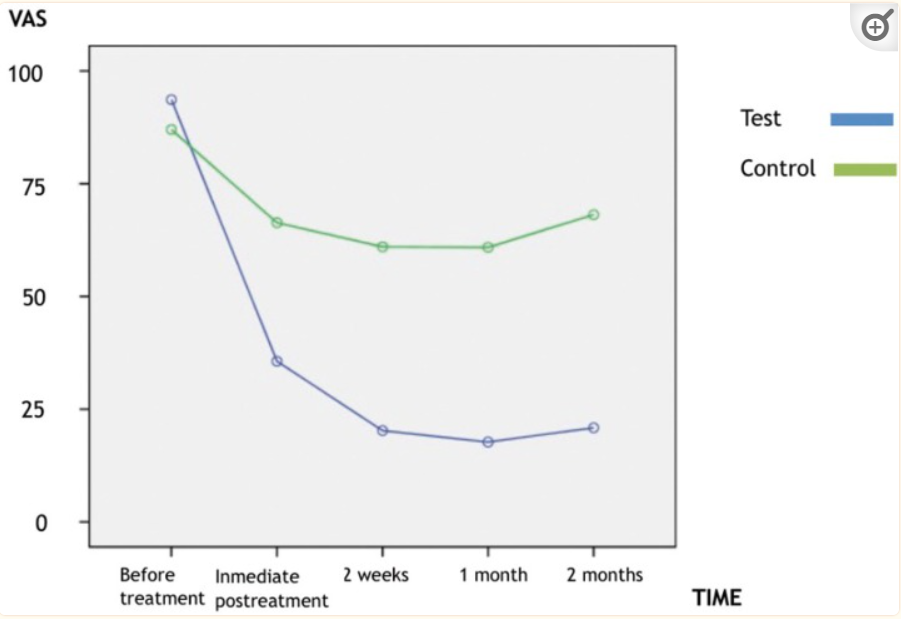
- And to thermal stimuli, in the same study:
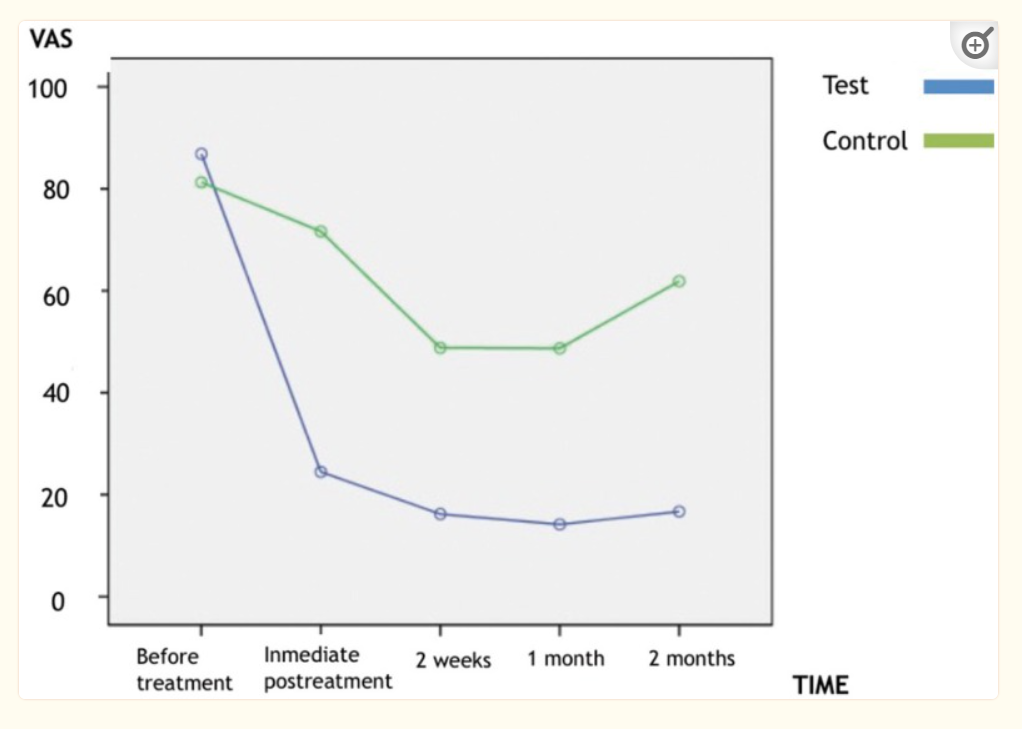
- Then, 810 nm and 1,064 nm lasers were compared to a desensitizing agent over 18 months (47). There were a few different groups, with both a lower-powered laser at 10 J/cm2 and a higher-powered laser at a 40 J/cm2 dose. Also, the 1,064 nm laser emitted 85 J/cm2. Some of the laser groups also received the desensitizing agent. Surprisingly, no difference in treatment effects was found, however!
- Moreover, another study an 810 nm laser with a desensitizing toothpaste, or both (48). The laser therapy group outperformed both groups in terms of pain after one week but that effect levelled off after three weeks.
- Next up, a 650 nm laser toothbrush outperformed Sensodyne toothpaste (49). The laser toothbrush led to quicker results.
- Then, a high-powered and low-powered 810 nm laser were compared to a desensitizing agent (50). The light therapy doses were either 10 or 90 J/cm2. Three treatments with lasers, with 72 hours in between them, led to dentin hypersensitivity relief for up to 6 months. Combining dentin desensitizers with light therapy led to the best results.
- Furthermore, a study used a 635 nm toothbrush or a very low-powered 635 nm toothbrush (51). The VAS scale (which measures pain from 0 - 10) in the intervention group was reduced from 5.8 to 2.3. In the control group, with the low-powered light, the VAS was reduced from 6.4 to 5.5. So the higher-powered device had a much greater result!
- One more interesting study used a 660 nm laser after a periodontal flap surgery - where gums are attached higher to clean the area below (52). One part of the mouth was treated while the other was not. Hypersensitivity and pain were reduced in the laser-treated part of the mouth. The only issue that I have with these "split-mouth" study designs is that there is likely a systemic effect of treating one area on the other area of the mouth.
- Moreover, a desensitizing agent was compared to placebo (a thickening gel) and a 780 nm laser (53). No difference was found over three months.
- Then, 810 nm (8.5 J/cm2) and 2,780 nm lasers (dose unknown - likely hard to test for!) (54). Both lasers led to less hypersensitivity.
- Next up, a study tests a laser against a fluoride agent and different controls (55). The laser group uses 810 nm at 8.5 J/cm2. Dentin hypersensitivity was measured for a period of up to six months. The fluoride worked initially but led to increases in the pain (VAS scale) after three and six months. The laser treatment maintained the achieved results.
- Another super interesting study compared 630 nm LED with 660 nm lasers and both worked equally effectively (56). There was a 30-day treatment period and 60-day followup.
- One more study on gum recession, combining 808 nm and a desensitizer agent, or just 808 nm alone (57).
- A surprising study outcome finds no difference between 660 nm laser treatment, a desensitizing gel, and a placebo gel (58).
- Then, an 810 laser was compared to a desensitizing gel, and a control group (59). It seems like the effects of the gel and laser weren't perfectly separated in the study reporting. There was a 36.9% reduction in dentin hypersensitivity 15 minutes after laser treatment. After 14 days, that number increased to 71.7%. After 60 days, the laser sensitivity reduction number was still 65.7%. These results are extraordinary...
- One study I wanted to include, even though it's not an RCT, is on the 660 nm and 830 nm comparison (60). 660 nm was more effective than 830 nm here. The power of the lasers were the same in the study.
- Another study used a 830 nm laser four times over eight weeks (61). Thermal sensitivity was reduced by 67% in the treatment group and 17% in the control group. Tactile sensitivity was reduced by 65% in the intervention group and 21% in the control group, after eight weeks. There were no adverse effects.
- In one more study 633 nm was compared to 633 nm and 1,064 nm at high power (62). The outcomes were about the same.
So that's all!
Systematic Reviews - Which Have The Best Level Of Evidence
Next up, I went through the systematic reviews. Systematic reviews are traditionally considered to have the highest level of evidence in medical science because they analyze and integrate all previous research.
Nevertheless, I chose not to rely exclusively on systematic reviews because I wanted to form my own opinion on this subject. Also, the systematic reviews published don't take the most recently published papers into account.
Nevertheless, let's look at the outcomes of the systematic reviews below. I've only included interesting information that I didn't already come across in the previous section.
The Benefits Of Red Light Therapy In Dental Practice In Review Studies
Next up, I include a few recent review studies. These studies will give you additional information. Reviews analyze and integrate previous studies into a new whole. For instance, 15 earlier individual studies can be analyzed and integrated into one summarizing review study.
Let's go:
Systematic Review 1
The first systematic review concludes that there are benefits of red light therapy for dentin hypersensitivity in the short, medium, and long term (64). The literal word for the long-term effects that is used is "persistent". Well, I'm not so sure about the persistent effects because the results may no longer be present five years later.
Now, what's interesting is the treatment protocol standard - or, rather, the absence of a standard. The researchers write:
"The interventions consisted of a diode laser [...] or a neodymium-doped yttrium aluminum garnet laser (Nd:YAG) [...] and were delivered using a wide range of parameters in terms of wavelength (630–1067 nm), output power (1.5–1000 mW), total dosage (0.1–300 J), energy density (2–100 J/cm2), exposure time (10–180 s) and number of irradiation sessions (1–6)." (64).
So, yes, there's no universal treatment protocol. And there are many unknowns yet, that are simply untested for. You don't know whether 590 nm works, for instance, or how well, if no study has investigated it yet.
But let's get back to business:
What's most interesting here is the effect size. That effect size measures how big the difference between the effect in the groups is. An effect size of 0.5 is a medium effect, for instance, and 0.8 for a large effect.
Now, here's where the magic starts. The short-term effect size was 1.09, which is bigger than "large". In other words, the treatment already had a very strong effect in the short term. Medium-term, the number rose to 1.32. And, long-term, that effect size came out at a whopping 2.86, which is enormous (64).
Red light therapy for dental hypersensitivity thus has an enormously strong effect. Hence, the words "game-changer" in the title of my blog. Lastly, the review also gives an interesting explanation of how this is accomplished - for the nerds among us:
"Although the biomolecular and cellular [Red ligh therapy] activities have not been entirely determined, there were three perspectives referring to different stages how [red light therapy] alleviates [dentin hypersensitivity]. First, [red light therapy] may immediately change patients’ self-perception by modulating neuronal physiology in terms of varying the axonal flow, cytoskeletal organisation, and adenosine triphosphate production in sensory nerves [...]. Second, the effect of [red light therapy] on inflammation may play a role in the interim alleviation of [dentin hypersensitivity] since studies suggested there is a potential relationship between [dentin hypersensitivity] and micro-inflammation within dentine-pulp complexes [...]. The third theory is more explicable for persistent [dentin hypersensitivity] relief, as light irradiation may help increase blood vasculature in pulp tissues and stimulate the viability of odontoblasts; they both contribute to the deposition of secondary dentine and reduction of dentin permeation [...]." (64).
As a result, light therapy for dentin hypersensitivity probably results in three stages, the short, medium, and long-term effects.
Next up, what's important is that a lower total dose of 2 - 10 J/cm2 generally works better than higher doses, of 40 J/cm2 or more (64).
Lastly, there are a few caveats though, that need to be dealt with in future research:
- There are not enough high-quality randomized controlled trials.
- Many studies has a higher risk of bias.
- The studies comparing light therapy with fluoride generally have the highest risk of bias.
- The age ranges of the study participants differ and are unaccounted for. In the future you may find that light therapy for dentin hypersensitivity works better for old people, or for young people instead!
- There's insufficient quantitative data available, such as the air plast on a sensitive teeth. With better measurements, outcomes could be mapped better.
- Lastly - a thing that I had noted as well - there aren't enough long-term studies on the topic. An example would be to look what happens over the 2-10 year period after a study. Of course, doing so is prohibitively expensive, and that's why it's not done yet!
This review is from 2021, as is the next one. So, the 2021-24 data aren't taken into account yet! Moving on:
Systematic Review 2
The second review looks at the immediate and 1-month results of red light therapy for dentin hypersensitivity (65). Due to the high risk of bias, only six studies were finally included here. Also, only comparisons between placebo and light therapy were included, so no comparisons of light therapy with desentization agents.
Here an effect size of 1.49 for pain immediately after treatment was found, which is very high. That pain was measured with the VAS scale I talked many times before about in this article. After one month, that effect size grew to 2.29. These are huge effects of red light therapy on dentin hypersensitivity, once again!
One study uses red at 685 nm, and the others use near-infrared light.
Now, if you want to understand an issue I have writing this article, here's what you can see in Table 3 of the full text of the study (66):
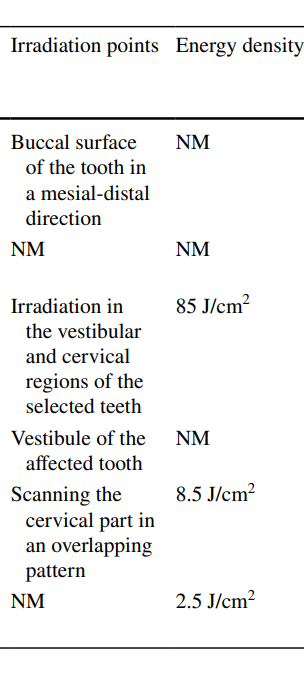
As you can see here, the light is applied to different regions. In some studies, the light is applied to the vestibule region of the tooth - the part that should be pink and holds the root of the tooth inside the jaw. In others, the cervical mid-part is treated, and in others it's different again. Also, the total dose in J/cm2 differs for each study, as is the wavelength, and so forth!
These variations in protocol make it very hard to recommend a universal protocol. Nevertheless, as you'll see, I will attempt such a thing!
What Other Human Studies, Animal, And In Vitro Studies?
I won't cover in vitro ("in the glass" - petri dish experiments like you did in chemistry class) here. The same is true for animal studies. Why? Simply because there's a wide availability of human studies right now.
Professional Treatments Vs At-Home Options
Well, if you want to eliminate all risks, by all means visit a dentist for your laser therapy treatments for dentin hypersensitivity. The biggest upside here is that you'll get someone with more experience who has done this before and can also access your teeth more easily.
A dentist can also help you distinguish between whether you've got dentin hypersensitivity, or another dental or oral problem that gives rise to the same symptoms.
And, for that last reason, I always recommend getting a dentin hypersensitivity diagnosis by your dentist first, before trying anything yourself.
At-Home Red Light Therapy For Dentin Hypersensitivity Device
So the device that I recommend, that allows you to reach many different areas in the mouth, is...
Stay tuned for it...
My recommendation is the LightpathLED Diesel Torch (code ALEX saves). I recommend this torch because it emits 660 nm and 810 nm, and has a high power output that approximates the laser studies. Also, the torch comes with a special oral probe, that allows you to specifically treat individual teeth, even at individual areas of these teeth. So, you can treat the crown, or the cervical area, or the root. The latter can be targeted by shining the light on the gums.
Keep in mind that to get a 2-10 J/cm2 dose, you'll only have to apply for seconds, often!
If you want more info, check Alex Fergus' LightpathLED Diesel Torch review. You can view a review of Alex's Diesel torch below as well:
Then, use the oral tip for the product to treat an individual tooth! You can either activate or deactive the blue light as well, with this device. Some studies have used blue light, as you can see above, so you may want to experiment with that!
Before I go into more data, let's consider a bit about the dosing:
Dosing
I recommend starting with the very conservative dosing protocol. The systematic review found a 2-10 J/cm2 to work best. From personal experimentation, I agree with that. With high total doses, sometimes my teeth became sensitive (normally they're not!).
Also, start slow. Monitor the outcome. If something isn't working, it's probably because something isn't working. And if something isn't working, you'll have to change things up. You may want to try an even lower dose at first. And, if a lower dose doesn't work, you can try a higher dose.
The LightpathLED Diesel Torch emits 100 mW/cm2 at the tip. This means that you'll have to apply the device for 10 seconds to an area of a tooth to get a 1 J/cm2 dose. And, per minute, you get a dose of 6 J/cm2.
So, applying the torch for 20 seconds gets you at the 2 J/cm2 dose that's the minimum in many studies. And, a 100-second application gets you all the way up to 10 Jc/cm2.
But let's say you wanted to experiment with a higher dose, towards the higher end that's used in studies, after you find out that the 10 J/cm2 dose doesn't work. You want to apply a 40 J/cm2 dose to the tooth. In that case, you'll have to apply the light for 400 seconds, or 8 minutes and 40 seconds, to achieve that 40 J/cm2 dose.
If you want to know more about dosing, just check out my blogs on the topic here:
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
Alternative Treatment Methods
Alternatively, you could use a handheld red light therapy unit or a tabletop panel to treat your teeth from the outside in. Our very own Alex Fergus has had great results with that method, because he noticed his teeth hypersensitivity went away after using red light therapy for the first time.
Nevertheless, here are some great suggestions for handheld units:
And, the same for tabletop panels:
For the best penetration, you'd need to use the skin-contact method, meaning that the light should be placed directly against the skin and jaw area. The problem here is that none of the studies use this specific dosing protocol.
But, I'd go slow at first, with a 10-20 J/cm2 dose directly against the skin at the chin and jaw area. Keep in mind that most light won't penetrate to the teeth even with this method, so you'll end up with a far lower dose at the root and cervical area of the teeth!
Again, there's no hard science on this topic so you'll have to use trial and error - and start slow!
Other Important Home Remedies for Dentin Hypersensitivity
Don't just rely on red light therapy - is my advice in almost any circumstance. Red light therapy should be part of a
Well, finding remedies for dentin hypersensitivity wasn't easy. I've searched for a few of the frequent areas which I tend to look in, and there's not even always evidence on these topics:
Common Lifestyle Interventions For Dentin Hypersensitivity
- For instance, we know that the circadian rhythm is extremely important for health. But, I cannot find any links between say, shift work, or circadian rhythm disruptions and dental hypersensitivity. For instance, there are huge changes in calcium and phosphorus metabolism with your 24-hour day and night cycle (17; 18; 19). Once this system is off, I hypothesize that it will affect dental hypersensitivity as well, as it does for almost any system in the human body. Calcium levels peak after meals and are generally lower in the late evening and at night. Phosphorus levels peak during the early morning and into the afternoon. Circadian rhythms are also involved in bone loss (20; 21; 22).
- Sleep quality problems are linked to poorer oral health (23; 24; 25). Yes, not a surprise because sleep quality is also linked to so many health outcomes. Poor oral health also affects sleep quality (26). But, no studies I could find between dental hypersensitivity and dental hypersensitivity. Exploring this topic is a no-brainer!
- No studies on magnesium, calcium, and phosphorus intake or supplementation and dentin hypersensitivity. Again, very sad if stuff like fluoride is extensively tested for, while the basics about natural prevention aren't even known!
- I've alluded to this before, but mouth breathing is strongly linked to poorer oral health (74; 75; 76; 77; 78). The mechanism is complex here though, and doesn't just involve acidity in the mouth, but also jaw development and structure.
Hydroxyapatite And Nanohydroxyapatite For Dentin Hypersensitivity
- Hydroxyapatite is the compounds that your enamel are made from. It's a calcium-phosphate and has gained popularity in natural health circles because it can remineralize teeth.
- Now, there are studies on hydroxyapatite and dentinhypersensitivity. For instance, a 2019 review (which analyzes and integrates previous studies) shows better effects of nano-hydroxyapatite for hot stimuli than cold, where old fashioned toothpastes outperform the former (27).
- A 2021 review shows hydroxyapatite stimulates dentine tubule occlusion and impedes dentin hypersensitivity (28). You'll need 2-8 weeks of treatment only!
- A 2023 split-mouth trial used nano-hydroxyapatite with pro-argin for the best results, compared to three other groups (29). Again, I don't link that they don't compare the (nano-)hydroxyapatite.
- In a 2022 study, a combination of zinc, magnesium, and hydroxiapatie won out, lowering dentin hypersensitivity in 100% of 10 participants (30).
- A recent 2023 review shows that hydroxyapatite has better outcomes for dentin hypersensitivity than placebo (31). Hydroxyapatite also works better than other densensitizers.
- Similar compounds such as biphasic calcium phosphate and oyster shell-derived nanohydroxyapatite may also work but are more poorly tested (32; 33).
Fixing Dental Related Issues For Dental Hypersensitivity
- Many other dental problems can cause dentin hypersensitivity, such as bruxism (teeth grinding) (67; 68; 69).
- Hard or abusive brushing may contribute to dental hypersensitivity as well (70; 71). Acids in the food may contribute as well, so don't keep them in the long too long (72; 73). Acid consumption raises dentin hypersensitivity risk by 2.72X, and swirling compounds in the mouth by 2.33X.
- Other factors may play a role as well. So get a 6-month checkup at the dentist at the very least!
Conclusion: It All Starts With Dentin Hypersensitivity Self-Care
Your daily habits determine a large part of whether you develop dentin hypersensitivity or not. Many of these habits are probably undiscovered, right now, and a few of them I've hinted at, such as your dietary intake and that of specific nutrients.
Then, there's simple oral hygiene such as brushing with (hopefully natural and remineralizing) toothpaste, flossing, regular dental checkups, and avoiding the worst problems (bruxism, excess sugar and acid consumption, etc!).
And then there's red light therapy as a game-changer! Almost anyone should use red light therapy as a tool in the toolbox, in this case!
Frequently Asked Questions
Does Light Therapy Ease Dentin Hypersensitivity?
Yes, there is overwhelming scientific evidence that even with just one treatment, most people decrease their dentin hypersensitivity. Over time, subjectively measured pain - so the pain that a study participant reports - can go down as much as 40-70%!
How To Apply Light Therapy For Dentin Hypersensitivity?
Right now, I recommend using a red light therapy torch. You can buy a torch online but I advice to get the LightpathLED Diesel torch.
That torch has an oral tip that allows you to apply the light therapy to a specific area of the teeth, with the dosing guidelines that I've established in the article I wrote on this article. The dosing will then accord to roughly the same parameters that were used in the science for dentin hypersensitivity self-care.
Is It Safe To Use (Red) Light Therapy For Dentin Hypersensitivity?
If you follow the scientifically directed guidelines in my article, and if you closely monitor your light therapy applications and reactions, you should be fine. But, to avoid all risk, always consult with your dentist before applying a dentin hypersensitivity home remedy.
Also, with tooth pain and red light therapy, make sure the dentist first rules out other causes before you continue. The same is true for dentin hypersensitivity medication interactions!
This is a post by Bart Wolbers of Lighttherapyinsiders. Bart finished degrees in Physical Therapy (B), Philosophy (BA and MA), Philosophy of Science and Technology (MS - with distinction), and Clinical Health Science (MS), has had training in functional medicine, and is currently chief science writer.
Items Mentioned:
- LightpathLED Diesel Torch (code ALEX saves)
Found This Interesting? Then You Might Like:
- Start Here - Light Therapy 101 & Buyers Guide
- Discount Codes, Deals & Recommendations - Red Light Therapy
- Red Light Therapy For Upgrading Your Brain Health
- Red Light Therapy For Sleep: The Science of Sweet Dreams
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studiespg