I know what you're thinking: "light therapy in periodontal care!? Don't I just need to brush my teeth and floss to maintain my gum tissue?"
Well, reality is quite different than the assumptions of you and me sometimes! And in this case, I'll explain how light therapy can really move the needle with regard to periodontal health. I'll also give you a few tools that may help enhance your results even further...
So why care about periodontal health?
The numbers on periodontal health are somewhat frightening. 90% of people have some inflammation in their gums (7). And 48% of people in the USA have chronic periodontitis - a chronic health condition affecting the tissues around the teeth (6). And 11% of the global population have severe periodontitis - with all of its negative health consequences (35).
I'll come back to that topic in a minute. But let's just say that many people aren't fixing their periodontal issues with just brushing and flushing. And what's worse is that this problem often progresses over time, without people knowing what to do about it...
Hence, a better solution is needed here!
Below, I'll explore topics related to light therapy for periodontal care. You can jump forward toward any topic you may want to read in the table of contents.
The topics I cover are an introduction to periodontal health, light therapy for non-surgical and surgical interventions for periodontal health, and finally, a section about other strategies you can apply to optimize this area of your health.
If you're short on time or just want to understand the basics, then read the summary below:
As an introduction, let's consider the anatomical structures and physiology first. Your teeth have adjacent tissues called the "periodontium." That periodontium includes not just the gums but also the bone in the jaw and other supportive tissues such as ligaments. You probably know that these tissues can be negatively affected in terms of health, and that's precisely what happens in gingivitis—inflammation of the gums.
In gingivitis, the gums are inflamed. Often, plaque also forms under the gums. Over time, if untreated and the situation becomes worse, the gum line can recede. Once that gum line recedes more than a few millimeters, you'll end up with "periodontitis". In periodontitis, part of the tooth is exposed that should normally be covered by gum tissue. In periodontitis, there's also space between the tooth and the gum, called a "pocket" - plaque and tartar can form there as well. Periodontitis is characterized by chronic inflammation but can also lead to further deterioration of the teeth and gums themselves.
So what's the fix?
Some factors, such as genetics and age, cannot be controlled, such as gingivitis and periodontitis. However, many other very important factors can be controlled, such as smoking, alcohol use, diabetes type II (which can be reversed in its early stages), visiting a dentist regularly for cleaning, and brushing and flossing your teeth.
Periodontitis isn't benign but can lead to systemic issues down the road! If you've got periodontitis, it will increase your risk of heart disease, stroke, Alzheimer's, cancer, and other conditions. Periodontitis is also considered irreversible, contrary to gingivitis. Nevertheless, dental treatments such as scaling and root planing can prevent further deterioration of periodontitis, because plaque and tartar is removed from the areas under the gums.
Now, here's where red light therapy for periodontal health comes in: about 70-75% of studies are positive when using red light therapy during these scaling and root planing procedures. These procedure are non-surgical and often performed at the initial stages of periodontitis. Right now, slightly more near-infrared studies are available here than red light. There is no universal protocol here, however, and the therapy is best applied by a dentist.
Next up, for surgical periodontal interventions by the dentist, studies are also generally positive for applying red and near-infrared light.
Unfortunately, there aren't too many studies focused at at-home use of red light therapy for periodontal health. Nevertheless, right now, I recommend using the LightpathLED Diesel Torch (code ALEX saves), which has an oral treatment tip. You'll have to treat each gum area for 50 seconds with the tip pressed against the gums for a 5 J/cm2 dose. That dose is very conservative and great for wound healing overall. Some of the studies also use light-emitting electric toothbrushes, which is where I base my dosing on. Please read my full blog post for more details.
Lastly, I want to clarify that I don't advocate focusing only on light therapy, dental hygiene, or dentist visits. Of course, these are all extremely helpful, but other factors, such as your nutritional status, your breathing habits, whether you smoke or not, drinking, and so forth, also determine your risk for gingivitis and periodontal disease!
Intro To The Periodontium And Periodontal Health
The "periodontium" is the supportive tissue around the teeth. That tissue includes the gingival tissue, the alveolar bone where the root of your teeth is placed in, and tissues in between the alveolar bone and the teeth (1).
Up to 90% of the human population has inflamed gums of some sort (1). Gingivitis occurs because bacteria and debris accumulate under the gum line - which eventually creates plaque. That plaque is a film on the teeth and under the gum line that can cause gum disease and caries.
Eventually, gum disease and disease of the adjacent tissues can develop into periodontitis. Periodontitis is a chronic health condition. The condition is characterized by chronic inflammation, as well as the slow destruction of the periodontium tissues. The immune system plays a significant role in periodontitis, as bacteria cause inflammation because of the immune response. That immune response, in turn, doesn't just target the bacteria but your body's own tissue as well.
In time, lots of damage to the periodontium can occur, leading to bone loss. Bone loss in the periodontium is often paired with bone loss in the teeth. Sometimes, this disease process can be really quick - such as if you've got a compromised immune system. In that case, there's so-called "necrotizing periodontal diseases". The gums rapidly deteriorate with necrotizing periodontal diseases, leading to bleeding, loss of gum tissue, and then further deterioration.
Different risk factors exist for periodontitis - some of which you can change and some of which you can't (2; 3; 4; 5; 6; 7; 34). Here are the factors that increase your risk:
- Tobacco smoking increases your periodontitis risk by 5 - 20X (7)
- Alcohol consumption and other substance abuse behaviors
- Other chronic conditions, such as osteoporosis and diabetes mellitus, and even mental health disorders in some studies! If you have type II diabetes, know that the condition is reversible in the early years, once you get your metabolism healthy again (8).
- Chronic stress (34).
- Genetics and age (which you can't change, unfortunately!)
- Pregnancy (yes, the women telling you their teeth went downhill with pregnancy are telling the truth!)
Then, the factors that decrease risk:
- Nutritional status, such as calcium and vitamin D, from diet and lifestyle (sunlight exposure).
- A healthy diet overall leads to a far better microbiome in the mouth, as well as a better interplay between the immune system and that microbiome (34).
- Regular brushing and flossing. In one study the risk of periodontitis is 4X lower with regular tooth brushing (5). Flossing lowers your risk by more than a third! I recommend a natural hydroxyapatite-based toothpaste if possible, without compounds such as SLS and fluoride.
- Visiting the dentists every six months at the very least, to remove plaque. Less plaque means less persistent bacteria, which entails
With time, inflammation in the gums and adjacent tissue can lead to loss of these gums. That loss determines the severity of the disease and is described the following way:
"The severity of the disease is based on the amount of clinical attachment loss (CAL). It is described as mild when the CAL is 1 to 2 mm, moderate the CAL is 3 to 4 mm, or severe when the CAL is more than 5 mm" (7)
Eventually, the periodontal disease progresses, and bone loss occurs. Then, the bone that holds the teeth and the ligaments around them are destroyed. Tooth loss can be the eventual end-stage, then!
Periodontal disease is not just a problem by itself, though. With periodontal disease, your risk of several diseases increases (8; 9; 10; 11; 12; 13; 14; 15; 16; 17; 18; 19; 20; 21; 28; 34):
- "all-cause mortality," or your overall risk of dying independent of cause by 46%
- diabetes and cardiovascular disease - with a 15 - 47% increase in a "coronary heart disease event" such as a heart attack with periodontal disease (depending on the study)
- stroke, in particular, cerebral ischemia, with a 60 - 330% higher risk with (severe) periodontal disease. The worse the periodontal disease, the higher the risk here.
- Alzheimer's disease
- adverse pregnancy events of 77%
- a few cancers, such as colorectal cancer (45%) and oral cancer, as well as overall cancers by 38%
- Rheumatoid Arthritis
- chronic kidney disease, where the risk in some studies is very small and in others by 100%
- respiratory illness
- And, most importantly, poorer overall oral health! So the worse your gum and adjacent tissue's health becomes, the worse many other issues in your mouth become!
Also, the worse your periodontitis becomes, the higher the risk of other diseases generally becomes (22). So let's talk about reversibilty. There are a few stages in this process (23; 24; 25; 26; 27; 28; 29; 30):
- Gingivitis is the initial stage of inflammation in the gums. You can simply see that yourself because you'll have red swollen gums, instead of pink ones. This gingivitis stage is fully reversible.
- Periodontitis is chronic for now, and not reversible. The bone in your jaw remodels in this stage, and is affected.
- Peri-implantitis is a condition in which the gum and other tissue around the implacts is affected. With bone loss and tooth replacements, you may need implants in your teeth, but these can be a source of problems as well. You may need implants once the periodontitis is very bad and your teeth start falling out...
- Tooth loss and toothlessness - if periodontitis is in the advantaged stages and the condition isn't prevented from progressing, tooth will become loose and fall out. Eventually, you could lose all your teeth and the structure supporting them. Implants are a great solution if you lose teeth, as they prevent further loss. Implants help maintain the structure of the bone. Toothlessness is not benign and is associated with about 30% higher overall mortality (your risk of dying of any cause).
Periodontal disease also affects quality of life, but that effect can be reversed with treatment (31). So, if you've got any gum issues, I hope I've convinced you an excellent strategy to start dealing with it!
So let's talk about the gum and adjacent tissue:
Just like the eyes, which I've extensively talked about in the past, the gums are also special tissue (32). Healing in the gums is scar-free, unlike in the rest of the body.
So, how is periodontal disease caused on a more microscopic level? Let's explore the following quote that nerds will like about the causes of periodontal disease:
"Putative periodontal pathogens are enriched as the resident oral microbiota becomes dysbiotic and inflammatory responses evoke tissue destruction, thus inducing an unremitting positive feedback loop of proteolysis, inflammation, and enrichment for periodontal pathogens. Keystone microbial pathogens and sustained gingival inflammation are critical to periodontal disease progression. However, recent studies have revealed the importance of previously unidentified microbes involved in disease progression, including various viruses, phages and bacterial species. Moreover, newly identified immunological and genetic mechanisms, as well as environmental host factors, including diet and lifestyle, have been discerned in recent years as further contributory factors in periodontitis." (33)
I'll return to many of these nutrition and lifestyle factors at the end of this blog. Suffice it to say that gingivitis and periodontitis are an interplay between microbes - including bacteria, viruses, and fungi - with your immune system and the overall milieu in your mouth.
Microbes significantly change in periodontal disease and their interplay with the immune system. Stress and diet also play a direct role in periodontal health. Prebiotic supplements can also be used, although that's a complex topic beyond what I'm trying to achieve here.
I'm oversimplifying here because the actual dynamic is complex - if you want to learn more, read my referenced review (34). Here's a fascinating infographic from that review, which I highly recommend you read if you want to know the ins and outs of the oral microbiome:
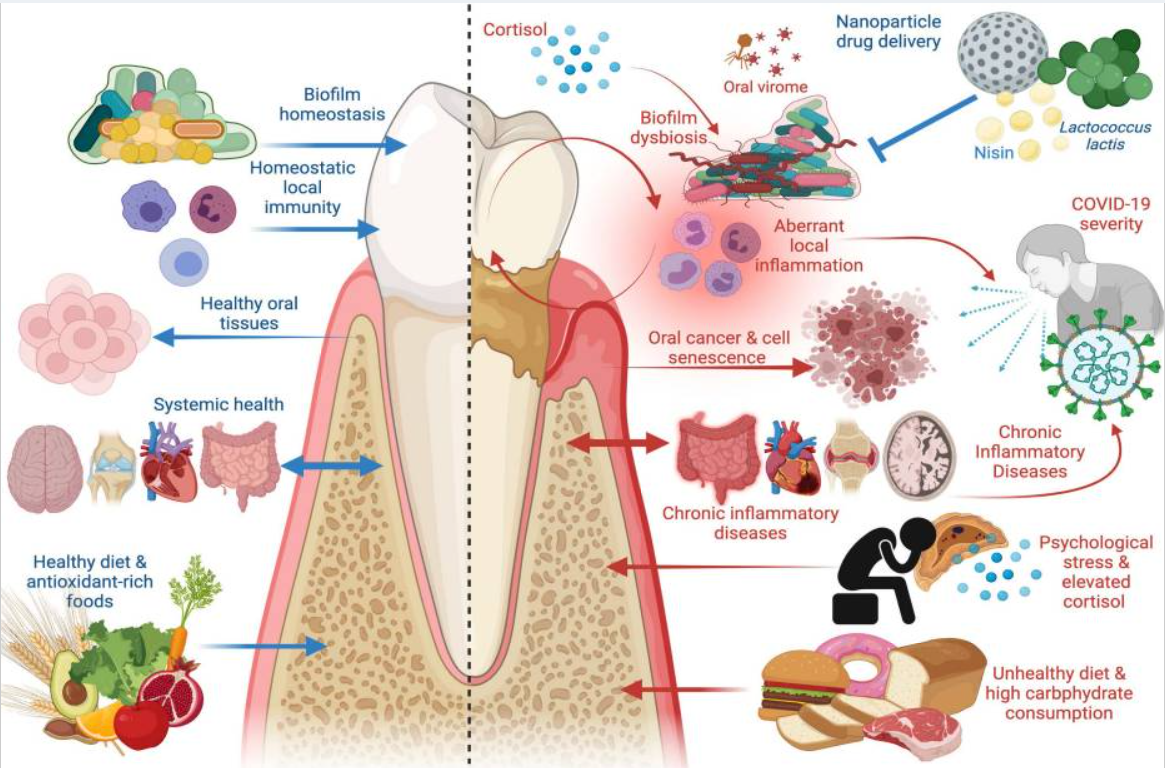
On the left, you can see factors promoting a healthy periodontium, while on the right, you see factors detracting from its health. So what happens if the periodontitis becomes really bad? You'll end up with periodontal disease and may need surgery, finally:
What Are Periodontal Dental Treatments And Periodontal Surgery?
So here I'll explore what periodontal surgery is (35). The goal is always prevention first, and preemptive treatment second, to avoid that surgery being necessary at all. Let's start with prevention:
Preventive Periodontal Dental Treatments
Two preventive strategies here are dental scaling and dental root planing. With dental scaling, you're removing the plaque and tartar (plaque that's hardened over time) from under the gumline. With dental planing, you're making the tooth root smoother so that the gum will reattach after plaque has been removed (36; 37; 38; 39).
These strategies are more important if your health is compromised, such as due to diabetes. New techniques for removing the plaque have also been developed (39; 40). Here's what a recent review states about this process:
"The success of non-surgical periodontal therapy is evaluated 6 to 8 weeks after scaling and root planing. This re-evaluation aims to identify any persistent signs of periodontitis, including ongoing gingival inflammation, deep probing depths, continued attachment loss, gingival recession, or worsening tooth mobility. Based on the concept of critical probing depth, probing depths of 5 mm or less at the re-evaluation stage should be treated nonoperatively. In contrast, sites with probing depths of 6 mm or more will likely benefit from periodontal surgery." (35)
So, losing gum tissue, having continued inflammation, or having the gum tissue not attached to the root of the teeth are all reasons to worry. If things continue to get worse, you'll have to consider the next step:
Periodontal Surgery
Once you get to the periodontal surgery stage, there are many, many options. I'll describe a few of these below - scroll down for a summary below if this part is hard to understand (41):
- Pocket reduction: here, the gums are lifted up, so that the plaque well below the gums can be removed. The gums are then re-attached to the bone. Normally, that plaque located very deep in the gums is not removable through the earlier preventive means.
- Gingivectomy: in this case, excess gum tissue is removed at certain places, which makes cleaning easier. Excess gum tissue is a problem for people who have their gums grown too far over their teeth.
- Gingival flap procedure: here, the gums are removed from the teeth and bone. Then, that part of that bone is removed. Next up, the gums are reattached but are now relatively bigger and better cover the area.
- Osseous surgery: in this case the tooth will also be reshaped, and plaque is removed from under infected gum tissue. The goal is to prevent further bone loss of the tooth and surrounding area. The bone is also smoothened out so that the gum better attaches.
- Bone grafting: here bone-like tissue is added, which can then support an implant. Sometimes there's too much bone loss in the jaw, for instance, to support the proper placement of implants. Bone grafting is then necessary as a prior procedure.
- Guided tissue regeneration: in this procedure bone-like tissue (a bone graft) is added, together with a membrane on that bone graft, which allows for better reattachment of the gum tissue to the teeth.
- Gum surgery for esthetical purposes: Many options exist here, and I just want to mention that fact, but I won't go into great detail here.
All of these procedures can have side effects. And, sometimes none of the procedures I've described above are useful, such as when the tooth loss is too big and it's better to remove the tooth altogether and think about other options. There's also often pain after these procedures, as they can be invasive (42).
So, next up, let's explore what light therapy can offer you in these cases - because some desperate help is needed to reduce pain and improve outcomes:
The Science Behind Light Therapy and Periodontal Health: Periodontitis And More
About 100 human studies on the interaction of light therapy and periodontium exist. Then, there are about 300 lab animal and in vitro studies. The latter is a petri-dish or laboratory design type of study that you may remember from science class in high school.
I'm using Vladimir Heiskanen's excellent Excel sheet with studies once again for this endeavor!
If you need an introduction into what these terms means, check the following resources:
- What Is Red Light Therapy?
- Red Light Therapy Explained: Basic Terms Guide
- Start Here - Light Therapy 101 & Buyers Guide
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
- How Often Should You Use Red Light Therapy Explained
These resources should give you a basic understanding of how red light therapy works, and the discussions around it!
Several topics exist here, but I'll first explore the most important one:
Light Therapy For Chronic Periodontitis
Below I've listed my analysis of all the human studies on light therapy and chronic periodontitis. If you want a summary, scroll down to the end of the section. But here's my breakdown of the human studies:
- One study used a laser at 2,780 nm near-infrared (or this could even be middle infrared) with patients who had at least 5 millimeters of "pocket loss" (43). "Pocket loss" means that the gum is no longer attached to the tooth for 5 millimeters more than normal, which is highly dangerous because it's a breeding ground for plaque and bacteria. The patients received scaling and root planing and medication to reduce the inflammation and redness in, their gums. Adding the laser reduced the depth of the pockets compared to the patients who didn't receive it and led to less bleeding of the gums. The light was applied every 6 months during treatment.
- Next up, a 1,064 nm laser was tested in diabetes patients and non-diabetes patients(44). Only in diabetes patients was there a result, and only in the short term. All patients underwent the non-surgical procedures of scaling and planing.
- Then, 940 nm light therapy at 3.76 J/cm2 was tested in patients with severe periodontitis (45). Light was applied three times in the first week. The outcome was measured after. Here, "plasminogen" was inhibited, which promotes inflammation and bleeding when it's available in excess. However, looking at the numbers, Heiskanen comments that there's no significant difference.
- One more 630 - 670 nm study saw no reductions in inflammation (measured by TNF-α) (46). The participants had pocket depths of 5 mm or more and some had diabetes. There was one treatment per week, after the scaling and root planing procedures.
- Another study uses 2,940 nm light and another undescribed wavelength (47). The scaling and root planing group, together with the 2,940 nm wavelength, worked best. Both probing depth (how far you can probe under the gum tissue) and the clinical attachment level (how high the gums attach) improved.
- Then there's a 630 - 670 nm study (48). Here, both the control and intervention group received scaling and root planing, but only the intervention group the light therapy. The calprotectin levels - which is a marker for inflammation - went down in the light therapy group.
- Next up, a 980 nm study with a monthly treatment for six months (49). A total of 30 patients had their 240 problematic periodontitis sites split up between ozone therapy and light therapy. Both ozone and light therapy worked for periodontitis, such as the pocket depth and bleeding, but light therapy outperformed after five and six months.
- A study using 380 nm to 1,400 nm, moreover, finds no results (50). There were four treatments over two weeks. Exposure was 20 minutes per site. No difference was found after three and six months.
- Furthermore, a study used 660 nm light for a 6.4 J/cm2 dose in people with type II diabetes (51). Treatment was every other day for almost three weeks. No effect was found in the light therapy group for periodontitis outcomes and glucose control.
- In smokers, 820 nm worked successfully as an adjunct in scaling and root planing (52). Pocket depth and clinical attachment levels improved.
- Next up, a study using 940 nm for 3.4 J/cm2 (53). Combining traditional periodontitis treatment with light therapy led to superior results.
- Then, a 940 nm study finds no effect on microbes when the pockets were irradiated with light (54).
- Another 1,064 nm study also finds no effect on the sensory system and blood circulation (55).
- A 645 nm study showed benefits only early on in the healing process but not later after three weeks (56).
- With 980 nm, moreover, with 7.65 J/cm2 applied three times over seven days (57). The pocket depth, attachment level of the gums, and inflammation all improved.
- Then there's a positive 810 nm light study (58). Again, there were improvements across the board, with better probing depth and clinical attachment level, and in the amount of bleeding.
- A 660 nm finds some benefit for medium-sized pockets (59). The light therapy group also had quicker benefits for pockets. There was one treatment at 22 J/cm2.
- Then, an interesting 660 nm study with daily treatment until 20 J/cm2 (60). This therapy was applied after scaling and root planing and led to a very positive overall recovery. Variables such as bleeding, clinical attachment level, pocket depth, and pain all improved.
- Next up, a study using 480 - 3,400 nm light to lower overall inflammation (61).
- A 980 nm study using 6 J/cm2 lowers harmful bacteria and showed improvements in the cell (62).
- A 940 nm trial, moreover, finds no positive outcome after three treatments in a week, after non-surgical procedure (63).
- Furthermore, a 1,064 nm study shows lower inflammation after just one session (64). The results were measured after six months.
- Then, a study uses 1.875 J/cm2 at 630-670 nm showed lower COX-2 expression - a gene associated with inflammation and immune system activation (65).
- An 808 nm study finds no effect at 4.46 J/cm2 with no positive outcome (66). There were three treatment sessions.
- Next up, a 980 nm study using 7.64 J/cm2 as a dose with good results (67). After three and six months, clinical attachment level, pocket depth, and the severity of gingivitis were all better in the light therapy group. There were four treatments in one week.
- Then a 685 nm study using just 1.6 J/cm2 also led to a reduction in pocket depth in periodontitis (68). The regular scaling and root planing were performed. Bleeding, clinical attachment, gum inflammation, and probing depth all improved more when light therapy was applied.
- Furthermore, a study using six treatments over six weeks at 810 nm led to improvements in periostin levels (69). Periostin is involved with bone remodeling and tissue regeneration. So theoretically, more optimized periostin levels should lead to better gum tissue health.
- A 635 nm study with three daily monthly treatments with an electric light-emitting toothbrush (70). Probing depth in the pockets decreased in the light toothbrush group versus placebo, as well as the clinical attachment level.
- Then, a 980 nm study showed almost no benefit of light application versus normal treatment (71).
- A 670 nm study shows a reduction in inflammatory biomarkers with either one treatment or with five treatments over two weeks (72).
- Next up, an 830 nm study at 3 J/cm2 reduced pocket depth (73). Bone density also improved over a 12-month period.
- An 808 nm study, moreover, using 4 J/cm2 shows improvements in periodontal healing (74). Here, bleeding, clinical attachment level, and probing depth all showed better results in the light therapy group than scaling and root planing only. Many biomarkers also improved. Light therapy may be especially useful in smokers, who much more often have periodontal disease.
- A 940 nm study, moreover, used the light in combination with methylene blue (75). That combination of light therapy with a substance that interacts with the light is called "Photo Dynamic Therapy" (PDT). The study showed good initial results for inflammation after one week and one month, but after three months, the intervention and control groups had similar results.
- Then, a 670 nm study with ten treatments over ten days (77). Testing the participants who received the light therapy after 1, 3, and 6 months showed less plaque, less bleeding, and less bleeding when probing.
- One study used 630 - 670 nm, moreover, the intervention group received light therapy five days in a row after periodontal treatment (78). Bleeding and the amount of plaque were less in the group receiving the light therapy.
- A 633 nm study had eight treatments over three months but didn't show any benefit (79).
- One more study with 630 and 780 nm also didn't show a result, but the total doses were very high (80). Well, 35 J/cm2 was used for pain with 780 nm and around 9 J/cm2 for healing (the latter number is reconstructed from the study and not written down). My interpretation here is that the analgesia goal interfered with the healing goal.
- And in the first actual wavelength comparison where 633 nm is compared to 650 nm, the results were more or less the same (81).
- In a split-mouth design, with light therapy applied to one part of the mouth while the other part doesn't receive any, 635 and 830 nm lower plaque, bleeding, and the depth of the dental probe (82).
- Lastly, a 635 nm study showed no results (83).
Systematic Review On Light Therapy For Periodontitis
In this section, I'll cover a few of the systematic reviews on light therapy for periodontitis. These review analyze and integrate many previous publications on a topic.
Often these reviews contain helpful information - and people writing them have spent tons of time researching this topic! These reviews also add another layer of rigor because studies are analyzed for conflict of interest, or improper reporting of the study findings, or other potential biases!
So here we go:
Review 1: Red Light Therapy Combined With Periodontal Therapy For People With Diabetes
This review study concludes that (84):
"[Red light therapy adjunctive to periodontal therapy in individuals with diabetes resulted in a greater reduction in probing depth and greater attachment gain in comparison to periodontal treatment alone (p < 0.05)."
So, overall, the gums will attach to the teeth better, and the gums will retain more volume so that the pocket depth remains smaller, with red light therapy versus placebo!
Good outcome! Only 8 studies were included in this review, however.
Review 2: Laser Therapy In Periodontal Treatment
The second review study also has a positive conclusion (85):
" [Red light therapy,] mediated by low-level lasers associated with non-surgical periodontal therapy, promotes additional benefits in the short term and accelerates the bone and gingival tissue repair process and also reduces postoperative symptoms of periodontal surgery."
The study does mention that there are no standardized protocols.
Review 3: Pain After Surgical And Non-Surgical Procedures With Or Without Red Light Therapy
The third review focuses on pain specifically and concludes (86):
"the alternative use of [high-powered lasers] to conventional instrumentation can significantly suppress postoperative pain and that intraoperative or postoperative [red light therapy] using diode lasers combined with periodontal surgery can significantly reduce postoperative pain. However, the evidence is still insufficient and more well-designed [high-quality Randomized Controlled Trials] are required."
So, there are benefits for pain after a periodontal treatment from the dentist, whether surgical or non-surgical!
Review 4: A High Risk Of Bias In Laser Therapy For Periodontal Non-Surgical Interventions
The fourth review aptly concludes the following (87):
"Current evidence lacks adequate information regarding the [red light therapy dosing parameters], which is fundamental in establishing a standardized and replicable protocol for future researches. Furthermore, substantial discrepancies in the study methodology and a high risk of bias, arising from the majority of the included papers, abet to the inferior quality of these studies. Ultimately, there is an urgent necessity to conduct further well-designed [Randomized Controlled Trials, the gold standard in Medicine,] in order to determine the effectiveness of [red light therapy], if any, by taking into consideration the abovementioned confounding factors."
So, researchers conclude that the risk of bias is very high in most of the studies I've analyzed. I'm willing to believe that immediately. Also, the same researchers state that the dosing parameters aren't listed well (or even measured), often, making studies impossible to replicate or interpret. I would agree with that assessment as well.
Nevertheless, I won't consider these studies useless. The fifth review has an interpretation that's much closer to mine:
Review 5: Red Light Therapy For Non-Surgical Periodontal Procedures
Here, in the fifth review, researchers state (88):
"Conclusion: This systematic review found that 70% of the included studies reported significantly better outcomes in certain clinical parameters, but no improvement in others. The remaining 30% of the manuscripts reported no significant difference in any of the measurements. With consideration to correct parametry, lasers have an adjunctive role in initial non-surgical periodontal therapy."
I'd also guesstimate a 70-75% positivity rate among the studies I've described above. And, contrary to the authors of review 4, I think many of these studies do show valuable insight, even if they're not fully free from bias.
Other Light Therapy Interventions For Periodontal Health
So, there are a few other studies that aren't related to chronic periodontitis but nevertheless concern periodontal health. I'll consider these studies below:
Light Therapy For Necrotizing Ulcerative Gingivitis
Necrotizing ulcerative gingivitis is an acute condition that develops much quicker than chronic periodontitis because of a bacterial infection (90; 91; 92). Ulcers and the dying off of gingival tissue are the result, combined with pain, bleeding, and overall systemic issues.
You're more prone to contracting this condition if you have a poorly functioning immune system. This form of gingivitis is extremely rare.
One case study investigated 980 nm at 9 J/cm2 on necrotizing ulcerative gingivitis,, describing how one human participant got good results (93). Pain was controlled, and wound healing improved, which led to an increase in quality of life.
Light Therapy For Aggressive Periodontitis
As you know, I'm following Vladimir Heiskanen's framework and he's allocated two studies under the header of "aggressive periodontitis".
One study shows that 980 nm added to the non-surgical periodontal procedures (scaling and root planing) leads to a smaller pocket depth, a better clinical attachment level, and a more favorable oral microbiome (94). Plaque levels didn't change.
Secondly, there's a 2018 review of light therapy for aggressive periodontitis that includes four different studies (95). Probing depth improved here while clinical attachment level didn't - the review states more high-quality research is needed!
Periodontium Biomarkers
Two individual studies can be found in this category, as well as one review.
The first study added 1.875 J/cm2 at 630 - 670 nm for either five or ten days to the non-surgical periodontal interventions. The non-surgical dentistry treatment caused a 31% decrease in inflammatory biomarkers, but with the light therapy, that number increased even more (96). The second study shows similar results, but doesn't give specifc numbers either, unfortunately (97).
The review includes 22 previous studies and concludes there is insufficient evidence for an effect, because studies vary too much in setup (98).
Gingival Hyperplasia
In gingival hyperplasia, there's an overgrowth of gum tissue (99; 100; 101). Hyperplasia can result from various causes, such as bad hygiene, medications, or just plain systemic health conditions. As a result, plaque may more readily accumulate, and oral hygiene becomes more difficult.
There's one case report on gingival hyperplasia - so with one participant - where 650 and 904 nm are used successfully (102). In this case, the problem was caused as a side-effect of medication use. After non-surgical interventions such as scaling and root planing, as well as antibiotics, it was the light therapy that finally lowered inflammation (103).
Gingival Inflammation
So the topic of gingival inflammation is probably most applicable to the average person. Why? Well, simply because gingivitis is so omnipresent in modern society!
There are four studies on the topic of light therapy for gingival inflammation:
- In one study, the intervention group used a toothbrush with red and white light, while the control group's toothbrush didn't emit any light (104). Bleeding was less in the group using the light-emitting toothbrush, but there were no statistically significant differences in plaque. Unfortunately, the study doesn't mention any of the treatment parameters such as wavelength or dose!
- Then, a case report of a patient with tooth restoration with resin, whereby 660 nm was applied at 35.7 J/cm2 at the soft tissue (105). Here, you can see the soft tissue around the tooth being treated - which later received a crown for aesthetical purposes (106):
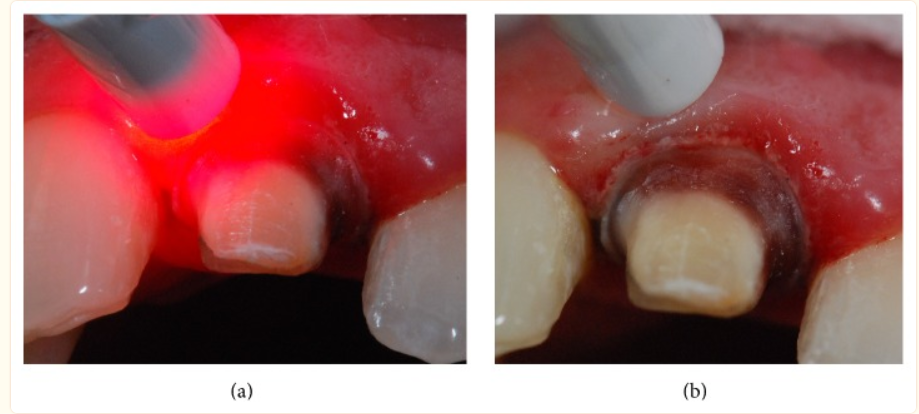
- As you can see in the picture above, the tissue around the tooth is really inflamed. After treatment and restoration, the tooth looks like this (106):

- A third study on gingivitis in children doesn't show any treatment data either (106). Light therapy resulted in quicker healing and less plaque
- Lastly, one study finds no effect of light therapy but doesn't really give any treatment parameters (107).
Overall, there seems to be a positive effect for gingival inflammation but more research is needed!
Gingival Lesions
One systematic review looked at gingival lesions because of autoimmune disease. The outcome here is that both pain and clinical scores for the lesions significantly improve (108). The "Visual Analogue Scale" (VAS) that measures pain from 0 - 10 has a 3.52 points reduction after 30 days and 5.04 reduction after 60 days.
Periodontal Implant Planning
Two different reviews investigate this topic (109; 110). The researchers state that due to the difference of treatment parameters in the studies, and their setup, it's not possible to give recommendations. Nevertheless, there are reductions in inflammation. There's healing of both hard and soft tissue.
Papilla Defects
Light therapy for papilla defects is also promising. The papilla is part of the developing tooth that later forms the dentin and pulp parts of the tooth. However, the word "papilla" also refers to the area between the tooth, that's frequently the source of cosmetic alternations.
In one study, the gingival tissue was provoked because a patient had an open area between the incisor teeth at the front of the mouth (111). Bleeding was provoked at the gum tissue here, and 635 nm light was then applied at the wound for 5 J/cm2, three times in ten days. After that, the area between the teeth got smaller (the "interdental papilla"), meaning that the gum tissue better filled up the area between the incisor teeth.
A second study used growth factors together with light therapy for the interdental papilla (112). The study doesn't show an outcome, unfortunately, and seems more of a proposal, but does show why this issue matters. Plaque control becomes harder with more space between the teeth, and jaw bone loss may result, so that dentists try to minimize this area between teeth.
Unfortunately, there's not a lot of research in this area yet!
Plasma Cell Gingivitis
In plasma cell gingivitis, the lower part of the gums is affected, closer to the jaw. Here a special type of gingivitis can occur, called "plasma cell gingivitis" (113). Here there's only one case study published (113). Bleeding - which is a frequent symptom of plasma cell gingivitis - stopped and remained absent for over five years.
Again, much more research is needed here!
Section Summary
Here's my summary of the current status of light therapy for the non-surgical periodontal procedures (by the dentist). I also explain at-home treatments:
,
There are slightly more near-infrared studies than red-light studies. However, the near-infrared wavelengths vary widely from study to study, so there's no universal protocol available here.
Unfortunately, moreover, there aren't many studies on the healthy gum tissue. Also, very few studies use at-home treatment right now, as opposed to therapy after surgical and non-surgical procedures carried out by the dentist.
So, How Can Light Therapy Be Integrated With Periodontal Surgery?
Periodontal surgery is very different from the non-surgical procedures I've talked about in the previous section. The dental scaling and root planing aren't surgical interventions - i.e., the dentist doesn't need to employ any invasive techniques that penetrate into your tissue, such as making incisions.
There are about a dozen plus studies on red light therapy after periodontal surgery. Here's the outcome:
- First up, a study after a surgical procedure called "open flap debridement". Here the gums are lifted and the area under the gums is cleaned, such as tartar buildup or infections at the root of the teeth. After the procedure, the gums are repositioned and stitched together. In this study, 890 nm was used three times in one week for pain relief and wound healing, but no differences were found between the intervention and control groups (114). Researchers measured many outcomes such as plaque, probing depth, bleeding, inflammation, and clinical attachment level.
- Then, a study using light therapy (unspecified) for gingival recession, with a graft from the patients' own tissue, didn't show any benefit from light therapy (115).
- A third study compares "Platelet-Rich Fibrin" (PRF) with 940 nm light therapy (116). Both interventions work equally well, although very little specifics are given about the light therapy once again.
- Next up, an 808 nm study shows benefits after the aforementioned "open flap debridement" surgical procedure (117). Light therapy caused less bleeding of the gums, a better pocket depth, and a better relative attachment level than not applying light therapy. Dentin hypersensitivity also decreased more with light therapy.
- A 790 - 810 nm study, moreover, shows no difference in pocket depth and clinical attachment level (118).
- Then, an 860 nm study shows a slight improvement in pain levels after three days, with three treatments in a week (119). This is after a "crown lengthening surgery", whereby either part of the tooth and/or the gumline is exposed so that restoration can be performed.
- An 810 nm study, moreover, compares light application or no light application combined with "Platelet-Rich Fibrin" (PRF), which I talked about before, for bone defects (120). Bone health, as well as gum health, improved when the light was applied. Pocket depth decreased with light therapy, as well as the clinical attachment level and the bone fill.
- Next up, a case report with only one human participant using 810 nm light (121). Here a coronally advanced flap surgery was applied. Here, the root of the tooth is initially exposed. The gums are surgically lifted for cleaning and then re-attached higher so that the pocket depth decreases and bone health problems of the teeth are minimized. The procedure was successful, although there's no placebo or anything else to compare it to!
- Furthermore, a 940 nm study finds that it reduces pain after periodontal surgery and that fewer painkillers are needed (122). A 20 J/cm2 dose was used after a periodontal flap surgery (once again to create larger overlap of gum tissue over the root of teeth). Here, one side of the periodontal area of the lower jaw area was treated while the other was not. Keep in mind that these results were achieved with one 2-minute laser treatment!
- Then, 1,064 nm was applied for so-called "furcation defects," which are bone loss problems in the area between the two roots of teeth, such as molars (123). The attachment level, as well as the probing depth of the pockets, improved more in the light therapy group, as well as overall bone structure!
- A study used 588 nm light for bone defects (124). Here enamel matrix protein derivative was used, which is a biologically active substance related to developing enamel. Enamel is the outer layer of your teeth, but the enamel matrix protein derivative can be used for regeneration. The light therapy reduced gingival recession, swelling, and pain compared to the control group that didn't receive light therapy.
- Lastly, there's one more study that doesn't show any results (125). No treatment parameters are given, though. Healing, pain, and bleeding didn't differ whether the light therapy was applied or not.
Light therapy ought to be integrated with periodontal surgery, although, the nature of the surgery and the application of light therapy varies wildly. Nevertheless, a majority of the studies have a positive outcome and none of them have a negative one. Different wavelengths and treatment parameters seem to work, but far more research is needed in this area, such as standardization of the treatment protocol and the concrete application of light therapy for different periodontal surgery procedures. Light therapy likely has benefits for pain, lowering the amount of gum recession, and the level of attachment to the bone and other structures.
Lastly, let's consider why you should be focused blindly on just light therapy and surgical or non-surgical interventions for periodontal health:
The Role Of Other Factors In Periodontal Health
Yes, I know you're getting bored with my approach. In almost any article I write, I talk about how health is multifactorial and why you shouldn't rely on just one health strategy to get the job done.
For instance, if you've got Alzheimer's Disease or the early stages of Mild Cognitive Impairment, I wouldn't recommend just applying red light therapy. I'd also recommend fixing your sleep quality, moving and exercising enough, cleaning up your diet, using targeted supplements, ensuring you're breathing correctly, and so forth.
Periodontal health is the same. Periodontal health is not just about applying light and going to the dentist. In the introduction, I've already mentioned that smoking alone increases your risk of periodontitis by 4 - 20X. Then there's alcohol use, and your overall brushing and flossing, and whether you regularly get dental cleanings, and so forth.
In this section, I'll look at a few other strategies you can apply to lower your risk of gingivitis and periodontal disease massively:
Nutrients
- Vitamin C status plays a very direct role in both gingivitis and periodontitis (126; 127; 128; 129; 130). Tons of research is available on this topic. People with periodontitis tend to have lower vitamin C status than people without - and may even have a lowered ability to absorb this vitamin. You'll need to consume at least 150% of the Recommended Daily Allowance (RDA) for the best results. However, once the damage is done, adding vitamin C doesn't help the results from periodontal surgery. Prevention is the best cure in this case! Chewing gum with vitamin C added, for instance, will lower the calculus formation (tartar that the dentist has to remove with specialized tools) by 33%. Bleeding sites are also reduced by 37%. Increasing vitamin C intake also helps reverse gingivitis. Adequate vitamin C intake alone is associated with a 12% reduced risk of periodontal disease (144). Vitamin C deficiencies are easy to fix by adding more fruits and vegetables!
- Vitamin D also plays a major role in periodontal health across the board (131; 132; 133; 134; 135). For nerds, here's what a recent review study (which integrates previous research) on the topic:
"Evidence suggests that low serum vitamin D is associated with increased severity of periodontitis, a chronic inflammatory condition characterised by destruction of the supporting tissues surrounding the tooth, which has several shared risk factors with other chronic non-communicable diseases. The biological functions of vitamin D are mediated by its strong anti-microbial, anti-inflammatory, and host modulatory properties. Experimental periodontitis models involving targeted deletion of 1α-hydroxylase, the enzyme responsible for the conversion of inactive substrate to active 1,25(OH)2 D3 (calcitriol), showed augmented alveolar bone loss and gingival inflammation. Vitamin D receptor (VDR) gene polymorphisms have also been associated with increased severity of periodontitis. Thus, the involvement of vitamin D in the pathogenesis of periodontitis is biological plausible. Clinical studies have consistently demonstrated an inverse relationship between serum 25OHD3 and periodontal disease inflammation. " (131)
- With Vitamin D (cont) there's a strong link to overall inflammation and immune system functioning, and periodontitis (132). And not only your periodontium but overall tooth health, such as the enamel, dentin, and even root, are affected by vitamin D–tooth loss or damage, of course, is related to periodontal problems once again! Periodontal treatment success also depends on vitamin D, whether it's surgical or non-surgical. If you want more info on how to create vitamin D through the skin, check the interview on the vitamin D lamp that Alex Fergus has carried out!
- Magnesium is strongly linked to bone health and also to periodontal health - although there are fewer studies as on vitamin C and D (136; 137; 138; 139; 140). Insufficient magnesium intake creates weaker enamel in the teeth and increases caries risk. Also, when increasing magnesium intake, probing depth (the depth of pockets, the loss of attachment of the gums to the tissue, and the number of teeth remaining goes up in older adults. More research is needed here but there's a negative association between magnesium intake and periodontitis risk. The people with the highest magnesium intake have a 31% reduced risk of periodontitis (139). In elderly smokers, you can lower your periodontitis odds by 5-6X with having the highest magnesium intake (140). These aren't perfect studies but hint at a strong link! Grab a magnesium glycinate supplement if you can't get sufficient from your diet - a powder is more economical if you're buying!
- Vitamin E likely affects periodontal health through many mechanisms (141; 142; 143). Evidence is relatively weak here though, but researchers write:
"The current literature suggests that vitamin E could improve the periodontal status by correcting redox status imbalance, reducing inflammatory responses, and promoting wound healing, thus highlighting the potential of vitamin E in the management of periodontitis." (141)
- Vitamin E (cont) is cheap and you can grab an inexpensive high-quality bottle from Amazon. Vitamin E is fat-soluble and can thus be stored–so taking a capsule twice per week under the tongue is sufficient! Higher vitamin E levels lead to a calculated (although imperfect) 13% reduction in periodontal disease risk (144). In another study, that number is 21% (145).
- Several B vitamins' statuses are linked to developing gingivitis and periodontitis–although research quality is low again (144; 145; 146). Taking a B complex supplement is linked to a periodontal disease risk reduction of 12% (144). In another study, that number is 18% for vitamin B6 alone (145)! Adding a B complex vitamin also improves the outcome of some periodontal surgery procedures (146). Vitamin B12, which you get from seafood and meats, may also be essential (147). Take a high-quality B-vitamin twice per week for the best results if your diet is poor.
- CoQ10 (Coenzyme Q10) is essential for energy production and levels tend to drop as you age. CoQ10 supports periodontal health across the board (147; 148; 149; 150). You can apply CoQ10 at the location where it's needed or systemically by taking a pill. Nevertheless, around half of studies show less pocket depth with CoQ10 administration (147). Other reviews show a decrease in plaque, bleeding, clinical attachment level, and pocket depth (148; 149). The best effect is achieved if the CoQ10 is applied near or in the pocket. If you're over 30 years old, I recommend taking the ubiquinol CoQ10 form daily. Adding CoQ10 helps achieve better results from the dental scaling and root planing (149).
- Omega 3 fatty acids, primarily found in fatty seafood, improve periodontal health as well (151; 152; 153; 154). In my opinion, after having read up on this topic for many year, fish consumption is superior to supplements here. Omega 3 fats have a low to moderate effect with benefits across the board, such as wound healing, pocket depth, and attachment levels.
- Zinc also has a significant effect on periodontal health although deficiencies are more rare here (155; 156; 157; 158; 159). The immune system, bone remodeling, and inflammation are affected by zinc. Zinc counters caries, gum problems, and bad breath, and may be a great additive to toothpaste (158). Zinc may protect people with type II diabetes against periodontitis (159).
- Lastly, calcium - here, the main point is that for proper bone structure, you need calcium. Without adequate bone structure, you won't only have tooth loss but also the adjacent structures (160; 161; 162; 163). Low dietary calcium intake increases your risk of periodontal disease by 84-99% (161). Simply including some dairy in your diet should fix your calcium intake. Fish (with bone) and green leafy vegetables are decent alternatives if you don't consume dairy for some reason!
My assumption here (I quote the research on this topic at other places) is that about 50% of people are vitamin D deficient, 75% magnesium deficient, 25% zinc deficient, 50% full-spectrum vitamin E deficient (although there's bad data here), and 75% omega-3 deficient (mainly EPA/DHA). B-vitamin deficiencies and calcium are more rare.
So, these nutritional strategies are extremely important if you don't follow a very good diet and get some sunlight frequently. I mention these because the statistical power of these nutrients taken together are extremely strong and can easily make the difference between having gingivitis or not, or having gingivitis regress into periodontal disease.
Other Strategies To Avoid Periodontal Disease
Here are a few other strategies you'll want to consider to decrease your gingivitis and periodontal disease risk:
- Mouth breathing changes the entire physiological dynamic in the mouth, such as the remineralization process through the saliva (164; 165; 166; 167; 168). Mouth breathing also affects how non-surgical periodontal interventions work, such as scaling and root planing.
- Platelet-rich plasma (PRP) - this is blood plasma derived by drawing blood from a person and then spinning it. That spinning separates parts of the blood, such as plasma, that can then be used for enhanced healing. Plasma increases wound healing and boosts tissue repair. PRP is traditionally injected at injury sites, such as an injured shoulder or a knee meniscus. Fortunately, PRP also seems to have a very strong effect on periodontal health, helping to regenerate tissue that would have been otherwise deemed "lost" (169; 170; 171; 172; 173; 174). The research currently doesn't reflect the things I've seen in clinical practice here - so if you need help, find a dentist that has applied PRP routinely!
- Tissue engineering - although much more research is needed here. Tissue engineering creates substitutes for original biological materials so that the tooth and tissues around it can function again. There's evidence this approach can work in the future for recreating bone, gum, and other tissue (175; 176; 177; 178).
- Be careful with alcohol consumption - this is somewhat of a no brainer, but there's a direct link between alcohol consumption and poorer periodontal health (179; 180; 181; 182; 183). Here's a good quote about that topic:
"Different alcoholic beverages in the market cause less salivation; these beverages contain sugars that promote acid production in the oral cavity by pathogens that demineralize the enamel and damage gum and teeth. This chronic alcohol consumption can progress into different types of oral disorders, including cancer, halitosis, and caries, and is also associated with tobacco and smoking. Chronic alcohol consumption can cause alteration of the oral microbiome and increase oral pathogens, which lead to periodontal disease and an environment of inflammation created in the body due to malnutrition, diminished immunity, altered liver condition, brain damage, and gut microbiota alteration. Heavily colored alcoholic beverages produce staining on teeth and, due to less saliva, may cause other toxic effects on the periodontium. Over-dependency on alcohol leads to necrotizing lesions such as necrotizing gingivitis, necrotizing periodontitis, and necrotizing stomatitis. These pathological impairments instigate severe damage to oral structures." (179)
- Alcohol (cont) - alcohol consumption increases periodontal disease risk by 25%, on average (180). Your risk increases by 0.4% for every gram of alcohol you consume each day (181). That's not the end of the world, but if you've got issues, you may want to take these factors into account. For each 300ml bottle of beer, there is a 6% risk increase.
Overall, I hope this section is clear: don't just focus on the obvious, such as dental hygiene and dentist visits. Lifestyle factors matter a lot for your periodontal health as well!
At-Home Light Therapy Use For Periodontal Health
So there's no easy answer here. Almost all of the studies I've covered - maybe except a few studies with a light-emitting toothbrush - use light therapy in a clinical setting under dentist supervision.
So how can you use red light therapy for periodontal health at home? Well, I'll have to become a bit speculative here. There's no hard science on this topic, but it does seem that lower total doses, such as under 10 J/cm2, work best generally.
To stay safe, I recommend a 5 J/cm2 dose at the gum tissue near your tooth. So if you've got gingivitis or a gum pocket at your incisors, or molars, or canines, you'd treat the gum tissue there for 5 J/cm2. And, to stay conservative, I'd recommend treating yourself three times weekly. Of course, all these numbers can change depending on the outcome you have - read my article about dosing to learn more.
So what device do I recommend?
As I described in my earlier articles on dentistry, I recommend the LightpathLED Diesel Torch here, because it has an oral tip that you can place on it. You can grab the LightpathLED Diesel Torch while using discount code ALEX to save.
If you want more info, check Alex Fergus' LightpathLED Diesel Torch review. You can view a review of Alex's Diesel torch below as well:
That torch has an oral tip specifically for dental treatment. That oral tip emits 100 mW/cm2 when you press it against tissue. So, you'll need to treat 50 seconds total for each location to get to the 5 J/cm2. Due to the small treatment area, you'll probably have to treat each gum area of each tooth separately.
Right now - although speculative - this is the best treatment protocol I can come up with, for at-home treatment of periodontal tissue. Hopefully, in the near future, we'll see far more studies in healthy participants or those with just gingivitis and home treatments. Heck, even people with severe periodontitis would benefit massively from studies that focus on home treatment instead of having to visit the dentist. And fortunately, there are more and more consumer market products available for this goal! So you've got more options than ever!
Finally, let's conclude:
Conclusion: Start Promoting Light Therapy For Periodontal Disease - Especially For Dentistry Treatments
Aw always, I'd love to see more data on this topic. Nevertheless, the science on periodontal gum care, recovery time for periodontal surgery, or even the implications on periodontal disease self-care, are already very promising.
I hope more dentists start applying photobiomodulation for periodontium care shortly. And, with more research and more standardization in the area, hopefully, you and I will learn more about how exactly light therapy is best used in this case and the benefits and downsides of different protocols.
The dozens of studies I've listed above are already promising. Since light therapy only takes one or two minutes to apply for many cases, dentists must get trained in this field and apply it to their patients if more research shows benefit. Given that light therapy is very cheap to apply once you've purchased a device, it's almost a no-brainer to integrate it more deeply into dentistry, in my opinion!
Frequently Asked Questions
Here, I answer a few frequently asked questions:
What Is Light Therapy, And How Does It Benefit Dental Treatments?
Red light therapy, in both the red and near infrared wavelength range, are helpful for both non-surgical and surgical periodontium treatments. You'll generally need a lower dose, of below 10 J/cm2, for better tissue regeneration. For full context, read my entire article though!
Is Light Therapy Safe For All Patients Undergoing Periodontal Surgery?
Yes, in the dozens and dozens of studies I've looked at, red light therapy seems safe for periodontal surgery. Of course, the light needs to be applied by a dentist, not by yourself. But, none of the studies I've quoted on red light therapy for periodontal surgery show any harmful effects - so an outcome where the intervention group is worse off than placebo.
Can (Red) Light Therapy Replace Traditional Periodontal Surgery?
Red light therapy cannot replace periodontal surgery, and cannot replace non-surgical periodontal treatments. For many treatments, such as the removal of calculus below the gums, or place a graft of tissue, or help the gums reattach.
Right now, red light therapy is only supportive of surgical and non-surgical periodontal interventions.
This is a post by Bart Wolbers of Light Therapy Insiders. Bart finished degrees in Physical Therapy (B), Philosophy (BA and MA), Philosophy of Science and Technology (MS - with distinction), and Clinical Health Science (MS), has had training in functional medicine, and is currently chief science writer.
Items Mentioned
- LightpathLED Diesel Torch - (code ALEX saves)
- Magnesium Glycinate Supplement
- Full Spectrum Vitamin E
- Ubiquinol CoQ10 High Absorption Form
- High Absorption B-vitamins
Found This Interesting? Then You Might Like:
- Start Here - Light Therapy 101 & Buyers Guide
- Discount Codes, Deals & Recommendations - Red Light Therapy
- Dentin Hypersensitivity: Why Red Light Therapy Is A Game-Changer
- How Red Light Therapy In Dental Anesthesia Practices Shows Great Promise
- Red Light Therapy Dosing: Why It's Complicated!
- Dental Red Light Therapy Before And After Case Studies From Clinical Practice









