Welcome to my second article on red light therapy for dental health. This time, I'll cover a super-dreaded topic for many people—getting dental anesthesia. Just the thought of a syringe going into your gum tissue is enough to make many adults afraid of dental visits. And let's not even begin with children!
If the amount of pain or even discomfort could be lowered significantly, I think modern dentistry could make great moves because more patients would come in for early treatment and wouldn't wait until problems have escalated. So, red light therapy for dental anesthesia is an extremely important topic because it can make the management of dental problems much easier in the long term!
If you're short on time, read the summary below. For the full details of my argument, read the entire article!
Anesthesia is essential for modern dentistry because otherwise we'd return to barbaric practices with lots of trauma and psychological stress. The problem, however, is that many people aren't comfortable with anesthetic injections themselves. Anesthetic injections are among the most frequent reasons people avoid dentists in the first place!
Just seeing the needle, let alone feeling it go inside the tissue, gives rise to anxiety and fear. Dentists have tried to solve this problem by applying anesthetic gel beforehand, distracting the patient, and so forth, but there no foolproof solution yet.
Overall, the effects of red light therapy for dental anesthesia injections are highly positive, with 20-40% reductions in pain in both children and adults. That pain is measured with a "VAS" scale, which measures pain levels from 0 - 100.
Looking at the published literature, the near-infrared wavelengths from the 800 nm and into the 900 nm range have the best level of evidence, and higher doses of 20-70 J/cm2 seem to have better outcomes than lower doses (5 J/cm2) and medium doses (10-15 J/cm2). About 80% of studies show positive outcomes in favor of the light therapy intervention over the placebo.
And, while this method isn't foolproof, the red light therapy for dental anesthesia does help a lot, especially if science can finetune the effects in the coming years.
There's less good evidence for using red light therapy for the duration and success of anesthesia, however. But still, in those areas, the studies are either neutral or positive, so no real risk is involved.
For anesthesia during dental treatment, I suggest using the device that your dentist is using. It's very hard to apply a device for the purpose of red light therapy for dental anesthesia yourself because the syringe is placed in a very specific location. Also, the dentist will determine where the anesthesia needs to be applied, so you cannot apply the light therapy yourself before a dentist visit.
Overall, this makes at-home treatments in this area very difficult. Nevertheless, light therapy for lowering pain before you get anesthesia is very promising with regards to the science and another area where light therapy applications shine bright!
Given the science right now, it's my belief that any dental practice should start implementing red light therapy for their anesthesia practices...
Introduction: The Convergence Of Dental Anesthesia and Red Light Therapy
In the last few years, there have been tons of publications on red light therapy and dental anesthesia. Generally, red light therapy makes anesthesia much less painful, and there are other benefits as well.
But let's first explore why anesthesia is such an important development:
Why Dental Anesthesia Is Necessary
You're pretty lucky going to the dentist today compared to 100 years ago. Anesthesia is arguably one of the biggest developments in the field of the last century. For most of humanity, the best any dentist could do for you was to have you take a few shots of strong alcohol or some other drug before a potentially painful dental procedure.
Nowadays, however, everything is different! Most dentist today apply local anesthesia when using any potentially painful dental procedure. Whether the dentist needs to drill, or whether you'll have your wisdom teeth extracted, or otherwise, not having to undergo the pain makes the dentist visit a lot more comfortable.
About 15% of the global human population has dental fear and anxiety - about 12% has high fear and anxiety, and 3% severe fear and anxiety (1). Sometimes, in some countries, these numbers are far higher though (3). Fear for the dentist makes people hold off getting treatments, often until there's a medical emergency and treatment can no longer be put off. Avoiding the dentist until it's too late also drives up the total healthcare costs (5).
For younger people, these numbers are generally worse. In some countries, 15% of children and adolescents are highly afraid of dentists (2). Other studies show a number as high as 30% for children (7). Dental fear is not just an abstract problem but affects the well-being and systemic health of children, in part because of dental treatment avoidance (4). Fortunately, there already are interventions to make children feel better, such as slow belly breathing when in the dentist chair (6).
But ideally, you'd like to eliminate dentist fear and anxiety for both children and adults. The problem here is that oral anesthesia is meant to reduce dental fear and anxiety--but is also itself a major source of dental fear and anxiety (7). Seeing the syringe and feeling it go inside your body are two major fears of people visiting the dentist, as are dental extractions.
Hence, better solutions are necessary. And red light therapy can play a major role there - as you'll soon see. But, let's first explore the topic of dental anesthesia itself:
Understanding Dental Anesthesia
Here's a very simple summary of a recent review on dental anesthesia - reviews aggregate and analyze previous research on a topic:
"Anesthetic agents work by reversibly binding to sodium channels, preventing the entry of sodium into the cells and thereby inhibiting the propagation of nerve impulses. Consequently, nociceptive impulses associated with painful stimuli do not reach the brain, and the patient does not perceive pain." (7).
The anesthetic agents are injected to affect the trigeminal nerve (8). That trigeminal nerve is one of the only 12 nerves that directly emerges from the brain, without interference of the spinal cord. You can see the trigeminal nerve here, and how its related nerves move towards the jaw:
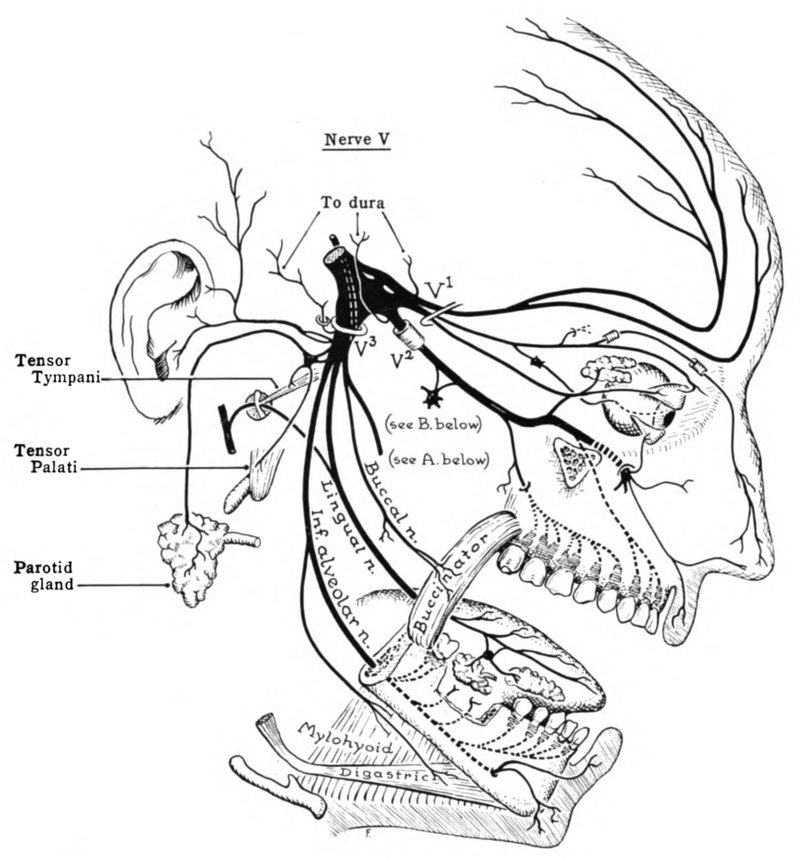
Both the upper and lower jaw are affected by that trigeminal nerve. And, by blocking calcium signaling, you thus stop any painful sensations from reaching your brain. Hence, you feel numb while otherwise painful dental procedures are carried out.
The anesthetic agent needs to be injected in the area where you need the anesthesia. For the upper jaw a more targeted approach is often used, while for the lower jaw which has a different structure, a broader approach affecting a larger area is commonly executed (8).
Now, the issue is that not everyone can receive anesthesia equally well (9). Kidney or liver problems, pregnancy, medication, heart and blood vessel disease, and age can all affect ability to apply anesthetics or its dose.
Next up, different anesthetic agents also have a different effect Here's a good quote about the pharmacology of differences of anesthetic agents:
"Local anesthetics are divided into two classes: amides and esters. Amide anesthetics are common in dentistry, including lidocaine, prilocaine, mepivacaine, and bupivacaine. Articaine is an amide anesthetic with an ester linkage. Ester anesthetics are less frequently utilized in dentistry, but drugs such as benzocaine may be used for topical anesthesia.
The gold standard and most widely used local anesthetic in dentistry is lidocaine due to its safety and effectiveness. Adrenaline is added to lidocaine to counteract its vasodilating properties and delay drug absorption, which prolongs the duration of anesthesia and reduces the toxicity risk." (9).
You probably know the feeling of anesthesia, at least, I hope you do! If not, you're either very unfortunate or fortunate (because you never had dental issues!). The anesthesia is applied to the inner cheek, palate, the oral mucosa, the teeth itself, the nerves in the jaw, or any adjacent regions! So, most of the oral region can be affected.
Anesthesia isn't without risk either. You can have allergic reactions, the anesthesia may not work for you, you may have bleeding or the injection may hit a blood vessel, overdose on the anesthetic agent, get nerve injuries, and more (10).
Nevertheless, anesthesia is essential to lower dental fear and anxiety for many visiting the dentist (9). Anesthesia isn't foolproof, however. Individual anatomical variation, or poor technique, are some of the reasons why anesthesia may not work as intended.
Fortunately, there are developments in dentistry anesthesia (11; 12; 13; 15; 16; 17). New anesthetics are used, for instance, such as electricity-based anesthesia, distracting the patient (yes, I've watched Netflix in Mexico during dental appointments!), vibration, cold applications, and more. This field is developing rapidly in the last few years. Potential side effects are also better dealt with through new methodologies.
So, finally, let's look at how red light therapy works for dental anesthesia - another field that has been massively improved upon in the last few years:
How Light Therapy Enhances The Effects of Dental Anesthesia
In this section, I go by the categorization made by Vladimir Heiskanen's Excel sheet with regards to oral health. Heiskanen categorizes studies according to analgesia in general, anesthesia duration, anesthesia injection pain, and overall anesthesia success.
Let's start with the first:
If you need an introduction into what these terms means, check the following resources:
- What Is Red Light Therapy?
- Red Light Therapy Explained: Basic Terms Guide
- Start Here - Light Therapy 101 & Buyers Guide
- Red Light Therapy Dosing Chart: The Raw Data From Hundreds Of Studies
- Red Light Therapy Dosing: Why It's Complicated!
- Red Light Therapy Wavelengths Benefits: The Ultimate Guide
- How Often Should You Use Red Light Therapy Explained
These resources should give you a basic understanding of how red light therapy works, and the discussions around it!
Analgesia In General
Here, three studies are included. I'll go over these studies one by one:
- First, one study compares 980 nm light to local anesthesia for fixing caries in children (18). A total dose of 21 J/cm2 was applied over four minutes. The total pain was measured by having the child select a face, that signifies the amount of pain they are having. The local injection outperformed the red light therapy slightly, although not statistically significant. That outcome means that you can expect applying the light to the teeth works equally as well as an injection! The study tested both strategies with the same child, but at different sides of the body. So if the kid had caries left and right, the injection may have been tried at the left side and the red light therapy at the right side.
- Next up, a review on red light therapy for dental analgesia (19). That review analyzes and integrates previous research. The biggest complaint here is that study quality is low overall. Four out of five studies showed positive outcomes, but couldn't be pooled together for statistics because the study setup varied big time from study to study. This is a complain that we've been seeing a lot more in the light therapy space - but is perhaps at least partially invalid because there are so many variables to test for!
- Lastly, another study on 1,064 nm in humans at 73 - 107 J/cm2 (20). The laser was compared to analgesic cream. The study participants needed premolar extraction, which are the teeth between your canines and molars. The dental pulp, which lays below the enamel and dentin layers, was effectively anesthetized with the laser, with slightly better results than the cream! The people who received the laser treatment didn't report any numbness either. Both electrical and mechanical painful stimuli were tested for, and suppressed by both methods.
Overall, these are great results for the analgesic effects of red light therapy!
Anesthesia Duration
Anesthesia duration is vital because some procedures take a long time. However, often the patient is left with a numb feeling in their chin, mouth, or related area for hours.
Hence, let's check the five studies that can be found on anesthesia duration and red light therapy:
- First, a study compared 635 nm and 808 nm in children (21). Here, 15 minutes after exposure to the light, 88% of people treated with 808 nm and 68% with 635 nm returned to normal sensation. After 45 minutes, all returned to normal and the pain was lower than in the control teeth/area (where a fake laser was used). High power levels were used at 400 and 500 mW/cm2. The problem here is that children often injure themselves, such as biting themselves in their chin, as a side effect after anasthesia.
- Another 660 nm had the same outcome, where anesthesia was minimized and the injury to soft tissues as well (22). Recovery of sensation was almost double as quick in the 660 nm group versus the control group.
- Then, one more 808 nm study used 11.5 J/cm2 and direct contact over a 23-second period (super high power!) (23). Two points around the injection site received light, as well as 10 points around the alveolar nerve. The aveolar nerve stems from the trigeminal nerve which I talked about before. The difference wasn't too big in this study, with 122 minuts of anesthesia in the laser group and 134 minutes in the control group.
- Next up, one more 660 nm and 810 nm comparison (24). The total treatment time was 72 seconds over six different points. 660 nm reduced anesthesia time by 34.7% and 810 by 27.6%. This outcome is contrary to the first study, surprisingly!
- Lastly, one study uses 810 nm only (25). Each lower side of the childrens' mouth either received a sham or a real laser. Return to normal took 145 minutes in the laser treated side and 188 minutes in the control side.
So far, so good! Seems like red light therapy can significantly reduce the duration of the anesthesia in children!
Anesthesia Injection Pain
There are 19 different studies on red light therapy for anesthesia injection pain. As you already know, the feeling of the syringe going into your mouth, or merely seeing the syringe, gives people discomfort or pain. Others already get discomfortable by the thought of having to go to the dentist and receiving injections!
Fortunately, some dentists use numbing gel before they inject the syringe into the oral tissue. Nevertheless, that numbing gel doesn't work on a very deep level and you'll still feel some pain in many cases.
There are 19 studies on anesthesia injection pain and red light therapy. I'll first explore the regular human studies (such as "Randomized Controlled Trials") below:
- First, 660 nm was used in children at 12 J/cm2 over one minute (26). So that's a 200 mW/cm2 dose! Both objective (heart rate) and subjective (selecting a face signifying pain or no pain, or in between) were used. Applying the red light therapy significantly reduced injection pain, as well as the heart rate of the children during the procedure!
- Next, 940 nm light was used with a strong laser (27). The dose was 10 J/cm2. All participants receiving the laser treatment had a "Visual Analogue Scale" (VAS) of under 3. The VAS scale measures subjective pain between 0 ("no pain") and 10 ("worst pain imaginable"). The control therapy was a fake laser.
- Then, 980 nm was used for 15 J/cm2 in children (28). Here too, the VAS score, heart rate, and the faces signifying pain or no pain, and everything in between, improved with the laser treatment. The results of the light therapy intervention were better than cold application, vibration, or local anesthesia.
- Then, an 808 study with just one participant but it did show a 50% reduction in pain (29)!
- Another 810 nm study finds no effect in children at 5.2 J/cm2 before injection, as well as local anesthesia (30). The control group only received the local anesthesia, before the injection, but no light therapy. What is interesting is that this study setup is different than the previous ones with reference number 26 - 29 that I discussed, in that here both groups receive the local anesthesia.
- One more study has a similar outcome but shows slightly better outcomes with a higher treatment time (31). Here, the 40s treatment time outperforms the 20s and 30s, with more people reporting "no pain". Overall injection pain didn't differ between the 20s, 30s, and 40s treatment time - at 940 nm!
- Another 940 nm study did show improvements with the laser therapy over just local anesthesia (32). The dose didn't matter though, as three doses were compared.
- One more 940 nm study finds that it does help over no intervention at all (33). The VAS score with laser was 2.1 and without laser just under 2.8. The dose was 15 J/cm2.
- A 915 nm study, moreover, finds a 2.5 VAS with the laser and a 4.3 VAS with the control laser (a sham laser that doesn't work) (34). A high dose of 72 J/cm2 was applied. Nevertheless, this is a huge difference in pain perception - as pain is reduced by 30% or so!
- Furthermore, a study used 808 nm at around 32 J/cm2 in kids (35). Heart rate and pain were significantly reduced with the light treatment versus anesthetic gel.
- Another study uses 980 nm in children with success (36). The average heart rate of the kids was lower, and they reported less pain when visually selecting the faces, and they made less sound and moved less in the chair with the injection.
- Then an 810 nm study using 69 J/cm2 in children in just 20 seconds (37). That's a whopping 3,450 mW/cm2 for power output - I wonder whether that's a mischaracterization! One side of the face received local anesthesia, and the other local anesthesia and red light therapy. The mouth part treated with light therapy showed 41.7% "no pain" while that number was 21.7% for the anesthesia only. Severe pain was 3.3% for light therapy and 11.7% for anesthesia only. So once again there's a huge difference here! The light therapy didn't affect injection efficacy either, which is quite important!
- Next up, an 980 nm study shows that the laser reduced pain, but that just a sham laser that doesn't work also reduces pain (38). The pain reduction with the sham laser wasn't as good as the regular laser though!
- A study using 660 nm, moreover, participants received a local anesthetic in their mouth as well as either an activated or deactiveated laser (39).
- One more study uses 810 nm before wisdom teeth removal at 67.5 J/cm2 over 30 seconds (40). Two points were irradiated with that light, twice over. The light therapy didn't decrease pain in this study, however, but did reduce heart rate of the participants.
- Lastly, there's a 790 nm study that doesn't show statistically significant improvement either (41). However, looking at the pain scores, the VAS score is lowest in the light therapy group, although the difference is not statisically significant, as mentioned earlier!
All of these studies are from the last ten years, so it's quite a new field! I'm very happy with this outcome as most of the studies show positive effects, and, the difference in pain and other outcomes can be huge often!
Anesthesia Success
So there are four studies on this topic:
- First, there's a 810 nm study that didn't show any improvements in the time it took for the anesthesia to work or how well it works (42). A dose of 15 J/cm2 was used over a 20 second treatment. The treatment was the dental pulp inside the tooth, that's really sensitive once affected because by then often the enamel and dentin layers have already been compromised.
- Next up, a 980 nm study shows benefit of not only minimizing pain but also the need for additional injections for anesthesia (43). The laser treatment only took 20 seconds but no dose was given (probably high-powered though like many of the other studies!) This study invoved a root canal treatment, where I'm generally more skeptical of as a long-term solution.
- Then, a 940 nm study at a dose of 78 J/cm2 (44). A difference was found here, but it was statistically non-significant. Here's what the researchers write:
"The no-pain scores of the experimental [light therapy] group were higher than those of the control group (29% vs. 20%). Moderate-to-high pain was more frequent in the control group than in the experimental group (43% vs. 20%). While 31% of the experimental group required supplemental anesthesia, 49% of the control group required supplemental anesthesia during pulpotomy of the tooth with [Molar Incisor Hypomineralization]." (44)
- Lastly, one more 940 nm study does show improvements in anesthesia success in people where the dental pulp is affected (45). The anesthesia success rate was 34% in the control group and 57% in the light therapy group!
Overall, we need more studies on the topic of anesthesia success and red light therapy. Some studies have a neutral outcome here while others have a positive one. Nevertheless, these results do look promising!
At-Home Light Therapy Usage For Toothaches?
So now the question arises, should you use an at-home device for toothache? I only recommend doing so for short-term pain management. You'll probably have to use higher doses of light, such as 20-40 J/cm2 at the very minimum and potentially going much higher.
What's known that in red light therapy for dental extraction, such as your third molars, red light therapy can have an excellent effect on painkilling (46; 47; 48; 49).
As I described in my earlier blog on dentin hypersensitivity, I recommend the LightpathLED Diesel Torch here, because it has an oral tip that you can place on it. You can grab the LightpathLED Diesel Torch while using discount code ALEX to save.
If you want more info, check Alex Fergus' LightpathLED Diesel Torch review. You can view a review of Alex's Diesel torch below as well:
Keep in mind you're using light therapy for pain and inflammation here, not for dental anesthesia. The problem is with using red light therapy for dental anesthesia is that only your dentist will be capable of knowing where exactly to place the syringe. So, only your dentist can apply the light therapy for pain at the exact injection location beforehand.
But, technically, you can use light therapy for pain management, if it's acute. The goal then is to lower your pain until you can go to the dentist. I don't recommend lowering your pain while never visiting a dentist. Of course, I recommend a more holistic dentist that doesn't apply fluoride, uses biocompatible implants (non-titanium) whenever possible, is aware of the dangers of root canal treatments, and so forth!
Still, if you use a LightpathLED Torch for impeding toothache, make sure to monitor your dosing during the process. You may need to increase or decrease the dosing or change the location that you're treating. There's no universal one size fits all when it comes to dosing.
But, with trial and error, you should be able to find out what works and what doesn't. Of course, if any protocol makes your tootache worse, then change things up. And, if a given protocol does work, keep doing it! Dosing can be that simple, really!
Also, you could theoretically use the Diesel Torch for painkilling after dental procedures. But I would recommend talking to your dentist about the exact protocol in that instance.
Are At-Home Light Therapy Devices Safe To Use for Dental Procedures?
Sure, at-home light therapy devices will be useful for dental procedures. But, knowing dentists, they will probably opt for more expensive lasers for their treatment, simply because they can apply tons of light to a tooth or gum tissue in a short amount of time.
So I wouldn't even use the LightpathLED device I've mentioned above in clinical practice. Of course, it's possible but it will take you a long time to apply the light, with 100 mW/cm2. Many of the lasers I've mentioned in the studies I've quoted above have up to 10X the power output, so you can easily get a 1 J/cm2 dose in a second and apply a reasonable dose in just 10 or 20 seconds of application.
With the hourly rate of dentists, it makes no sense to use the LightpathLED device in clinical practice. Of course, these companies fully know that and have developed these products as a safe option for the consumer market. Technically, though, if your dentist is skeptical about the effects of red light therapy for pain, they could always invest a small amount of money into a LightpathLED device, try it, and then decide to get a laser product that can often run into $10,000 USD.
Nevertheless, I recommend you visit a dentist if you have dental pain or in another area surrounding the mouth or jaw! Don't wait with treatment, as things can sometimes already have deteriorated over time before the pain finally has set in!
Conclusion: Dental Anesthesia And Light Therapy Is A Winning Combination!
The results in this area of using light therapy for anesthesia are absolutely wonderful. And, for me, it's just a knowledge-gap for many denstists as to why they don't apply light therapy for anesthesia yet.
There are several advantages, in my opinion:
- The light therapy can be applied super quickly if you have a higher-powered laser.
- The light therapy reduces stress and discomfort for the patient, making the entire dental procedure easier.
- The light therapy reduces stress and discomfort for the patient, making the dentist more relaxed in their work.
- The light therapy for anesthesia procedure looks to have a strong effect.
- The light therapy is super cheap to apply, once you've purchased the device.
And, sure, training and the initial purchase of the device are two big downsides of this application. But, applying light therapy by dentists is probably pretty easy in comparison, given the complexity of the procedures they're used to apply on a daily basis.
So, using light therapy in anesthetic applications has huge promise in my opinion!
Frequently Asked Questions
Here I consider a few frequently asked questions on this topic:
Can Red Light Therapy Replace Dental Anesthesia?
Theoretically, red light therapy can replace some parts of dental anesthesia, but I think they work better together instead of viewing them as an either/or relationship.
So, for the best results, you'll apply red light therapy and superficial anesthesia to a location first. Then, you use the syringe to fully remove all pain and sensation from that area. Your dentist should know how this process works.
If you still have pain, ask for more anesthesia! Suffering isn't necessary. And, if your dentist doesn't want to give anesthesia or doesn't want to give you more during a procedure even though you still feel pain, fire them!
How Long Does It Take To See The Benefits of Light Therapy After a Dental Procedure?
Generally, you'll have extremely quick results with red light therapy after a dental procedure. I didn't cover this topic in my article, however, and will come back to it in a later article!
This is a post by Bart Wolbers of Light Therapy Insiders. Bart finished degrees in Physical Therapy (B), Philosophy (BA and MA), Philosophy of Science and Technology (MS - with distinction), and Clinical Health Science (MS), has had training in functional medicine, and is currently chief science writer.